Centralized operations yields efficiency upgrade

Technicians in Banner Health’s remote operations center supporting their internal customers while implementing prescribed energy-saving measures.
Image courtesy of Banner Health
Seven years ago, Banner Health, a Phoenix-based nonprofit health system serving patients in 32 hospitals across six states, identified a big opportunity. It had implemented retrocommissioning at several of its facilities but saw potential for savings deteriorate over time because of changes and overrides made to its building automation system (BAS).
About the project
Winning entry
- Organization: Banner Health, Phoenix
- Project: Data-driven facilities operations initiative.
- Start date: January 2015.
- Completion date: August 2021.
- Budget: Minimal to reduce operational spend.
- Actual cost: Primarily operationalized spend.
Project team
- Mark Barkenbush, vice president of facilities services.
- Phil Dague, executive director of facilities operations.
- John Miller, senior director for facilities operations.
- Shawn Mathiesen, senior construction project management consultant.
- Brandon Conway, senior manager for remote operations center.
- Derrick McCloud, building automation system (BAS) analyst.
- Emmanuel Toth, BAS analyst.
- Burt Waite, president of Burton Engineering.
- Glen Anderson, president of ETC Group.
- Kip Edwards, former vice president of facilities services.
- Dan Dupaix, former senior engineer for design and construction.
- Sean Greer, former senior director for remote operations center.
Challenges maintaining operating room temperature, humidity and pressure requirements followed. Its decentralized efforts in previous years were triggering other significant negative consequences, too. It was time for a more efficient strategy and operating model that swiftly and successfully leveraged the organization’s scale and skills.
Banner Health embarked on a data-
driven facilities operations initiative in 2015 that aimed to consolidate decentralized technology, processes, procedures and policies; implement monitoring-based commissioning; merge computerized maintenance management systems (CMMSs) to a single platform; and develop universal protocols designed to improve building equipment operations. It would accomplish these goals and others by creating an innovative remote operations center (ROC) and forming a highly skilled team that, together, have decreased energy spending by nearly $12 million per year.
But these achievements paid off in more ways than bottom-line savings. For its exemplary efforts, Banner Health won the American Society for Health Care Engineering’s 2021 Excellence in Health Care Facility Management Award, which recognizes individuals or facilities management departments that implement new or innovative programs or processes to optimize the physical environment and improve patient care.
Tracing the timeline
Shawn Mathiesen, CEM, construction and engineering senior consultant at Banner Health, explains that the organization was at a crossroads a few years back and needed a better strategy to improve facilities operations.
“Monitoring and maintaining critical spaces is challenging for all major medical centers. We needed a standardized approach to not only ensure regulatory compliance but to optimize environment of care areas as well as enhance patient safety, efficiency and operational responsiveness,” he says.
Previous efforts through retrocommissioning and other energy initiatives resulted in high levels of savings drift across three to five years.
“We recognized that we were making facility-level decisions, not system-level decisions, and we didn’t have the team or expertise that could support each facility as a dedicated full-time equivalent (FTE) employee,” Mathiesen says. “That’s when we determined that changes were needed, including the creation of a new, centralized ROC.”
Adding extra pressure to this initiative was the fact that Banner Health was expanding, most notably via a merging in 2015 with the University of Arizona Health Network in Tucson; eventually, the health system would serve patients in facilities spanning Arizona, California, Colorado, Nebraska, Nevada and Wyoming.
“The growth and diversity of Banner Health facilities challenged our leadership in 2015 to explore a more efficient facilities organization and operating model,” says Mark Barkenbush, vice president of facilities services for Banner Health. “This ultimately led to a centralization of facilities operations in 2017 organized by geographic area rather than the previous model, which was a more siloed, single facility-based approach.”
In 2015, the organization began alpha and beta testing a monitoring-based commissioning program at two Banner Health facilities, the findings of which suggested this would be an effective strategy. Buoyed by those desirable results, the facilities management team launched Phase 1 of this program across one-quarter of its hospitals (recently, it completed Phase 4).
But the centerpiece of the organization’s initiative to shift facilities management practices to data-driven decision processes was the development of the new ROC and dedicated team, which started in 2015. Two years later, the ROC was up and running.
“Originally, we didn’t have the expertise in-house, so we partnered with a vendor that played a much heavier role in the beginning,” says Brandon Conway, CEM, senior manager for the ROC. “But we later agreed that our team would do some of the ROC creation work internally because it was a much more sustainable model for us long term. The organizational design of our ROC team included building management system technicians, coordinators and energy analysts that today has grown to a group of 12.”
Before the centralization of the ROC, each facility was acting as an independent department working with local staff and focusing on local issues, repairs and initiatives.

Remote operations center technicians cross-checking local chiller data against the building management system to ensure data integrity.
Image courtesy of Banner Health
“The consolidation of technology, policies, processes and procedures allowed our teams to create universal protocols to ensure the best approach was applied to the operation of all building equipment. This ensured that we could more easily identify anomalies in equipment operations across our facility portfolio,” says John Miller, CHFM, CLSS-HC, senior director of facilities operations for Banner Health.
“A great example of a big issue that all of our facilities faced was chiller surging,“ Conway says. “Through many conversations with the various manufacturers and engineers to identify the key characteristics for early identification and through proving the concept through several model iterations, we can now accurately predict a chiller surge before it occurs.”
Addressing other priorities
Aging infrastructure and critical utility infrastructure projects were high on the to-do list as well. Using data gathered from the centralization of its facilities operations department and implementation of the ROC, the team was able to secure a dedicated budget for a systemwide infrastructure renewal program.
Meanwhile, Banner Health had to address another serious impediment to progress: multiple BAS, CMMS and preventive maintenance (PM) tasks being used across its network of hospitals. Before long, it began consolidating and supporting software to enable centralized maintenance and compliance activities and unified processes and procedures.
“As we continue to grow and bring other hospitals into our system, we convert them over to our new consolidated systems, policies and procedures within the first few months of operation,” Conway says. “And, for our BAS platform, we’ve converted to an open-ended and nonproprietary version of Niagara building management software. Standardizing on the Niagara platform allows Banner to align all our sites with a standard sequence of operations, hardware and graphics. This standardization reinforces best practices and ensures data consistency.”
However, the push for progress didn’t stop there. Banner Health also worked hard over the past seven years to standardize contracts, improve building management system and construction standards, fine-tune precision PM tasks and procedures, increase regulatory compliance and transition more efficiently to updated operation plans.
“This is the beauty of fostering a culture of continuous innovation and improvement. We are not afraid to admit when something is wrong or needs tweaking, and our team works together on it to figure out how to solve the problem so that everyone can benefit — patients, visitors and staff alike,” says Phil Dauge, executive director of facilities operations at Banner.
Conway echoes those thoughts. “Our culture from the top down resonates continuous improvement with a strong focus on our patients. Our facilities operations department continually strives to do better for the benefit of our patients and staff, and our ROC and the centralization of our department is an extension of that.”
Fruits of their labors
Banner Health’s efforts over the past several years weren’t foolproof or without setbacks, of course. The ROC team encountered difficulty implementing standardized engineering and operational practices, achieving consistent communication with all facilities, and with manufacturers balking at service contract liabilities and limitations.
Despite these challenges, what the organization was able to accomplish is impressive, especially considering its size.
“We learned that, when we centralize and standardize on data-driven decision-making processes, we can create a significant benefit for the communities we serve, which is the ultimate goal,” Miller says. “We found that with the right team, including key internal staff assigned to the project as well as crucial external vendor support, our initiative could be successful.”
In particular, the gathered unified data allowed the team to observe trends at the system level, empowering them to make better-informed decisions and work toward a common cause. “These are issues that every hospital and health system are struggling with today,” Conway says.
Banner Health’s focus on using data to drive decisions has significantly increased staff productivity and efficiency.
“We have decreased diagnosis and repair times, decreased the number of hot and cold calls due to advanced analysis and remote resolution, and allowed for expertise in advanced control system logic to be housed internally,” Miller says. “We have also been able to reduce deferred maintenance and repairs using data and collaboration.”
Banner Health has shared its lessons learned and paths to success with other health care organizations. “What we’ve told them is that the effort to get to the finish line requires an awesome team. It also demands a well-designed plan based on data that can be sold to senior leadership — a plan that can and will change as variables are firmed up. Above all, the effort must be a collaboration, not an edict, in which every involved party is encouraged to provide feedback and suggest improvements,” says Phil Dague, RPA, executive director of facilities operations.
’Greatly impressed’
Gary Hamilton, PE, LEED AP, FASHE, the Arlington, Va.-based chair of the task force that chose the 2021 Excellence in Health Care Facility Management Award, says Banner Health’s project ticked all the boxes as a top-class submission.
“We were greatly impressed by their ROC and their ability to manage and augment different tasks, from maintaining equipment and ensuring energy efficiency within a building to commissioning and monitoring,” Hamilton says. “The ROC really pushes the envelope when it comes to what a systemwide control center should look like and how it should perform. It needs to be nimble enough to expand to other facilities, which is exactly what Banner Health did.”
He notes that being short-staffed and needing to operate facilities remotely were major challenges faced by hospitals during the pandemic, as was the ability to proactively monitor every patient room and temperature setpoints to reduce nuisance calls.
“Banner Health overcame these and other challenges with their facilities operations initiative and ROC, which they replicated across several facilities. In my several years of judging this award, this was one of the strongest submissions I’ve seen,” Hamilton says.
Barkenbush commends everyone involved with the initiative. “I’m so proud of the innovations my team has implemented over the past few years. We have made a positive impact on our patient care environment and our bottom line,” he says. “The recognition by ASHE of this work confirms our belief that we are on the right path.”
Conway adds, “Seeing our program mature year over year while continuing to improve patient care and yield energy and operation savings is extremely gratifying. Getting our facilities colleagues in the field to acknowledge our efforts is icing on the cake.”
Importantly, the initiative meshed with and supported Banner Health’s mission statement: Making health care easier so life can be better.
“It all ties back to providing a safer, healthier and better patient healing environment,” Miller says. “If our team wasn’t laser-focused on this mission, we may have each had great ideas, but we would have been running in different directions.”
Exceeding performance objectives through remote operations center
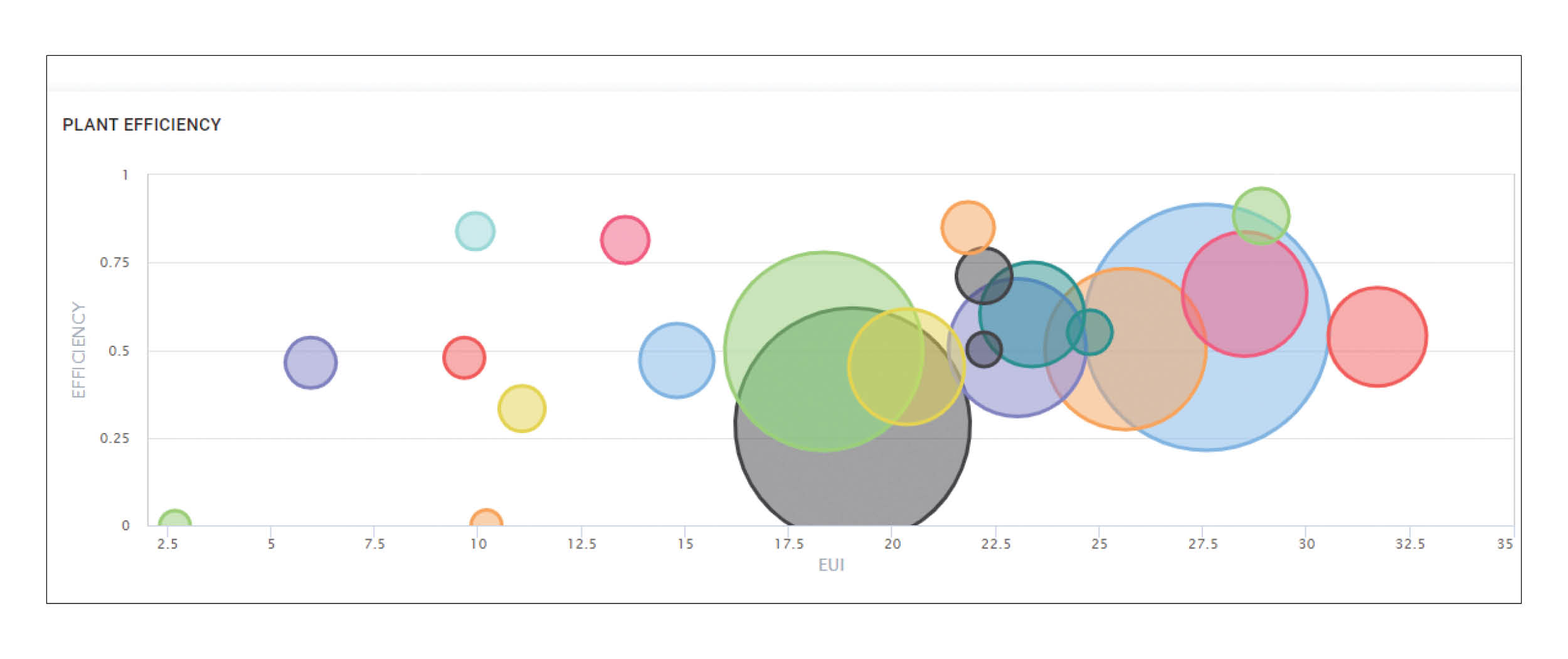
From the start of its initiative, Banner Health, Phoenix, identified areas of improvement and set ambitious objectives, including collective energy cost savings across its facilities.
“We as an organization continually set goals for ourselves and our team for each effort that we take on. These include a graduating scale of minimum to maximum performance expectations,” says Shawn Mathiesen, CEM, construction and engineering senior consultant at Banner Health. “Remote operations center (ROC) goals have been addressed annually when evaluating our performance improvements and have continually met or exceeded expectations.”
To improve Banner’s operating margin through cost savings, it created adjusted energy value targets: $0 to $1.4 million in annual energy savings was judged as not meeting the goal; $1.4 million to $1.7 million didn’t fully meet the goal; $1.7 million to $2.053 million met the goal; $2.053 million to $3 million exceeded the goal; and greater than $3 million in savings greatly exceeded the goal.
It’s safe to say that the latter target has been reached: Since 2016, the ROC team has reduced annual energy spending by almost $12 million. And every year, the ROC team avoids $3.85 million in utility spend drift alone made possible by continuous monitoring of faults and performance anomalies across systems.
The new ROC also has met or exceeded patient healing environment aspirations, including proactive monitoring of patient room temperature setpoints to ensure a comfortable environment of care; aggressive measures to reduce health care-associated infections via operating room and negative pressure isolation room dashboards containing real-time pressure, humidity and temperature data; and lowering avoidable operational spending by monitoring key building equipment to predict failure before it occurs.
“Our outcomes have far exceeded original expectations and have delivered a unified team with a single focus on utilizing data to drive decisions and improve the performance of our facilities services,” says Phil Dague, RPA, executive director of facilities operations. “The ROC specifically has become known as a systemwide resource whose expertise is used by our front-line teams, finance, construction and anyone else looking for answers to questions that were never readily available before.”
Erik J. Martin is a freelance writer based in Oak Lawn, Ill.