2025 Hospital Construction Survey results

Image for Getty Images
After months or years of construction, eye-popping budgets and countless planning meetings, the phrase health care facilities managers should hear on the Day 1 opening of a new project should be “Ready, set, go!” and not “Ready? Oh no!” But achieving operational and survey readiness on Day 1 is an issue that many health care facilities professionals continue to grapple with, according to the new 2025 Hospital Construction Survey.
Conducted by the American Society for Health Care Engineering’s (ASHE’s) Health Facilities Management magazine, the survey of hospital and health system managers and executives who oversee construction projects delved into the barriers facilities face in accomplishing Day 1 readiness, as well as the best practice contract requirements and internal policies that ensure facilities start operations well. The survey also looked at the current top construction, services and equipment project types; how planning, design and construction (PDC) budgets are faring since last year; and current barriers to completing PDC projects on time and on budget.
The stakes of a construction project meeting its operational obligations and regulatory requirements on its opening day are extremely high, says Chad Beebe, AIA, CHFM, CFPS, CBO, deputy executive director, ASHE Regulatory Affairs.
“It’s crucial that our facilities are fully prepared. While it might be Day 1 for the organization, for the patient, it isn’t. They deserve the same quality of care on the first day that they would receive if the organization had 400 days of experience,” Beebe says. “Something as simple as not having your air-handling unit balanced properly could negatively impact a lot of patients. Same with not being in compliance with fire or life safety requirements.”
Ready on Day 1
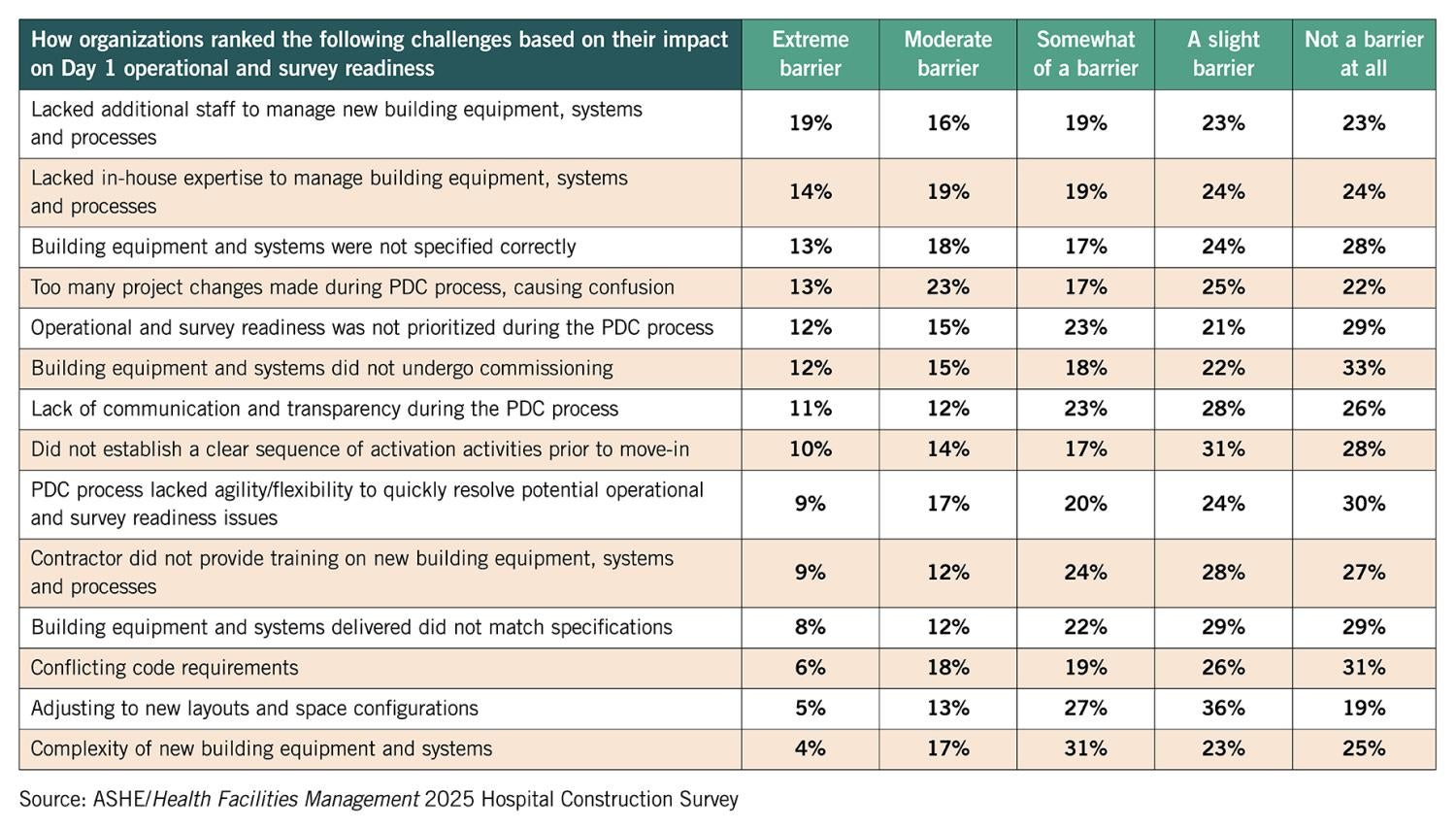
A best practice for being ready on Day 1 is commissioning, Beebe says. Survey respondents agreed, with nearly 80% saying they commissioned health care facilities projects — with fire safety systems, building automation and control, and electrical systems ranking as the top three commissioned building equipment and systems in new construction, renovation and expansion projects. Ideally, Beebe says, that figure should be closer to 100%. Cost cuts to keep projects on budget is likely the barrier, but the value proposition of commissioning needs to be better highlighted by facilities managers for senior leadership, he says.
“These systems are all complex — you need to commission the system to make sure it functions as it was designed. You want to make sure you get what you paid for,” Beebe adds.
The only way to be sure a new building, renovation or major equipment system functions as intended is to test it — and commissioning provides that test, says Dennis Ford, MHA, CHFM, CHC, FASHE, director of corporate facilities management support at Atrium Health and ASHE president-elect. Given the stakes, health care leaders can’t afford to skip commissioning, he says, especially with the increasing complexity of many building infrastructure systems and their interconnectivity making it impossible to get by with just individual component acceptance testing. “We need to show that our systems can maintain temperature, humidity, filtration rates, air exchange rates, etc., and we cannot show that without systems integration testing and documentation,” Ford says. “Without proper commissioning, you’re sunk.”
To ensure they are ready on Day 1, survey respondents said they craft internal policies and practices at their hospitals. The top three: Building systems and equipment training (79%), staff building tours (64%) and performing emergency management drills and exercises (57%).
Also, 58% of survey respondents said they build operational and survey readiness requirements into their PDC contracts with third-party contractors. The top three contract requirements were building systems and equipment training (83%), holding meetings with the facilities management team throughout the PDC process (77%), and building systems and equipment commissioning (76%).
Getting facilities tours throughout the PDC process and proper training by contractors — and sometimes equipment manufacturers — on key systems and equipment are vital to ensuring health care staff is ready on Day 1, according to Jonathan Flannery, MHSA, CHFM, FASHE, FACHE, senior associate director of ASHE Regulatory Affairs.
“Contracts need to state what type of training is provided, who will provide that training and when the training will take place,” Flannery says. “Training ensures facilities staff can operate the physical environment properly and provide the appropriate standard of care, and tours show the folks who will maintain the building how it was put together — which is extremely helpful even years down the road. As an example, if staff are still trying to figure out how to manage the water system properly on Day 1, patients could be exposed to waterborne pathogens and be susceptible to health care-associated infections.”
Lacking additional staff or in-house expertise to manage new building equipment, systems and processes were identified by the survey as top barriers to projects being operationally and survey ready on Day 1. The best way to combat staffing and resource challenges is preparation, Ford says. Before Day 1, facilities managers should fully understand how to operate new equipment and know the areas it serves, build an approved maintenance program, schedule preventive maintenance with current manpower and understand the probability of failure for each critical building system component. “We need all of this information to put together a maintenance strategy and staffing plan, and that all has to be done before Day 1,” Ford says.
Another barrier: facilities teams getting to weigh in on new projects too late in the process. The best way to tackle several of these issues, Beebe says, is advocacy.
“Facilities leaders need to start advocating for education early in the process. You can’t wait for the ribbon-cutting ceremony to learn how to operate a new facility,” he says. “Everyone in the hospital is struggling with having enough skilled staff to complete objectives. You have to advocate for your staff and their needs, lay out the value proposition and communicate what would happen if that system goes down in numbers or risks that senior leadership can understand. For example, [regarding] airflow, if you can’t maintain pressure relationships and this piece of equipment fails and the surgery area is shut down, what is the financial impact?”
Projects are “survey ready Day 1” when facilities managers and PDC professionals build a bridge of communication and understanding of their respective roles, priorities and operational, regulatory and policy requirements, Ford says. To have those conversations, facilities managers need to be at the table from Day 1 of planning a project, not just Day 1 of opening it.
PDC budgets on the rise
More money is expected to be allocated to health care PDC projects this year, with many survey respondents saying they expect an increase from 2024 to 2025 for new hospital construction (46%), renovation (59%), infrastructure upgrades (61%) and off-site facilities projects (44%).
Hospitals and health care systems are finally starting to get their financial and operational footing following the COVID-19 pandemic, leading once-shelved PDC projects to move forward, according to Mark Howell, a Seattle-based senior vice president at construction company Skanska. An increase in patient demand also is driving forward more projects, he says.
“There’s certainly a high demand for health care — we have an aging population, and people are staying in the hospital longer, so we’re seeing an increase in the number of planned bed towers,” Howell says. “There were several years where most of the health care system was just trying to recover from COVID-19, and now we’re starting to see that turn around and more projects that have been on the table for a while becoming reality.”
Facilities renovation projects saw the highest jump among PDC types in the survey in terms of what percentage of their organization’s capital budget is allocated to construction projects. In 2024, respondents estimated 30% of their hospital’s capital budget would go to renovation projects, but the actual number averaged 35%. Respondents estimate that number will be around 37% for 2025, another increase.
The desire to build more and newer health care facilities as well as renovate and improve current locations for both staff and patients may be due to hospitals looking to claim more of the market share and attract new patients in an increasingly competitive environment, says Angela Mazzi, FAIA, FACHA, EDAC, principal at GBBN Architects.
“As health systems start to merge, they overlap catchment areas, and patients in general are more consumer-driven. It is critical that health care is easier to use and access,” Mazzi says. “We also have staff shortages, so health care organizations have to think about what amenities, state-of-the-art services or technologies will bring staff to work in one location over another. This is driving the construction of newer buildings and the renovation of existing facilities to expand services, attract staff and create patient loyalty by delivering a value-driven and convenient health care experience.”
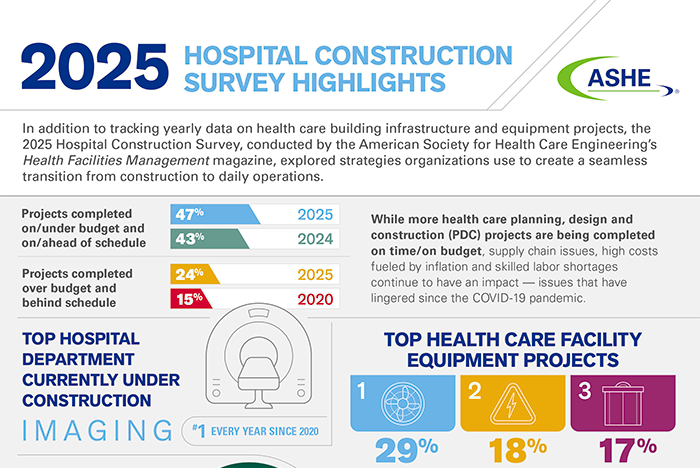
While more health care PDC projects are being greenlit, the field’s ability to deliver them on time and on budget is still somewhat of a mixed bag. A total of 47% of respondents reported that their PDC projects are being successfully completed on/under budget and on/ahead of schedule — up from 43% last year. But 24% said projects are both over budget and behind schedule, up from only 15% reporting the same challenges in 2020.
Though the worst of it seems to be leveling off, the lingering effects of the pandemic are to blame for project problems, Howell says, with supply chain issues, high costs fueled by inflation and skilled labor shortages continuing to haunt the field. “Also, a lot of construction and equipment businesses didn’t survive the pandemic, so you have to find replacement companies to work with,” Mazzi says, which can add time to projects.
To deal with these issues, many have been employing workarounds to keep projects on track. For example, Mazzi and Howell say many are turning to prefabrication and modular components for things like heating, ventilating and air-conditioning (HVAC) projects or mechanical and electrical systems, which lower costs and smooth out timelines through better labor utilization. Larger health systems have seen savings by creating design guideline documents that standardize common elements of a project, Mazzi says, like the look of exam rooms or the finishes in facilities.
To get around the exceedingly long lead time on electric switchgear due to supply chain issues, Ford says his team recently decided on the size and type of switchgear for a new hospital prior to finalizing the design drawings to ensure the equipment would arrive on time. “And then we had to ensure our design fit that gear because if you change your mind, you go to the end of the line,” Ford says.
Top projects for 2025
Since 2019, the survey’s No. 1 project type currently under construction has been acute care hospitals. But the number of projects has been on a rollercoaster since 2019, likely fueled by the pandemic. The percentage of respondents who were planning acute care hospital projects in the next three years increased from 16% in 2019 to 34% in 2022, only to drop back down to 20% this year.
“This is a ripple from COVID-19. In 2022, those acute care projects were addressing shortfalls found during the pandemic and working to have flexibility to address another pandemic,” Beebe says. “I’ve heard from other hospitals that they are now waiting to make those COVID-19 changes and opting to consider them further down the road.”
For top services and departments currently under construction, imaging remains at No. 1 on the survey — a spot it’s held since 2020. While imaging is a growing service in the health care field, ASHE experts say the likely reason imaging has remained on top is due to rapidly developing technology in this field, which is driving facilities to install the latest and best imaging equipment available.
“There is always a new imaging process or better way for getting imaging — kind of like your personal computer; if you don’t get a new one every three years, you are out of date,” Flannery says. This “march of technology” also is likely behind building controls topping the list for building technology systems for the last five years (24% noted this is currently under construction at their facility in the 2025 survey). Better automation of building controls can lead to extensive cost savings, especially in things like HVAC operations and lighting, ASHE experts say.
Air handlers topped the 2025 survey for currently under construction with 29%, followed by electrical switchgear/transformers (18%) and elevators (17%). That air-handler projects have held the survey’s top spot for five years is not surprising considering their upgrade was a key response to the pandemic, Flannery says. “Those are not easy to do; you are replacing an air system that you are running 24/7. And because of the complexity, those projects are extended out. We will probably see that same drive for five more years,” he explains.
It is similarly complex to replace electrical switchgear, which is a project hospitals often push to deferred maintenance. The rise of this and other infrastructure projects on the survey, however, could be the result of the increased emphasis ASHE has placed on developing deferred maintenance strategies and doing the analysis needed to determine when to replace critical systems, Flannery says.
According to Hospital Construction Survey data tracked from 2017, when ASHE published its pivotal “State of U.S. Health Care Facility Infrastructure” monograph, to the present, there has been a larger percentage increase in spending on capital infrastructure compared to spending on new construction over the same period.
“This shows ASHE’s advocacy efforts around deferred maintenance and paying attention to your critical infrastructure are having an impact,” Flannery says.
Notably, behavioral health department construction has fallen out of the top five for currently under construction projects after making the survey’s list from 2020 to 2022. Behavioral health departments were high on the list for “planned in the next three years” in 2022 but didn’t result in more projects under construction in 2023 or 2024. The reason for this could be hospitals innovating the way they deliver behavioral care, Mazzi says, working it into multiple services versus housing it within its own department.
“Health systems are asking, ‘What are other ways we can deliver that care? Can we embed it in primary care settings, or do more telehealth?’ Because while demand for behavioral health is continuing to increase, it doesn’t have the support of solid revenue. So, it is being built into existing service lines or supported with team-based care,” Mazzi says.
Click here for a downloadable infographic illustrating key results of the 2025 Hospital Construction Survey.
Related article // Special training needed for health care contractors
Another way to help ensure a planning, design and construction (PDC) project is ready on Day 1 is to hire general contractors who are knowledgeable about working in the unique health care environment.
Many managing PDC projects require contractors to hold health care credentials and certificates, like the American Society for Health Care Engineering’s (ASHE’s) Certified Health Care Constructor and Certified Health Care Physical Environment Worker, as well as get special education like infection control risk assessment (ICRA) training.
“When I was a practicing architect and served as a state authority having jurisdiction, time and time again when I saw new construction or major remodels go bad, the common thread was that the contractor wasn’t experienced in health care,” says Chad Beebe, AIA, CHFM, CFPS, CBO, deputy executive director, ASHE Regulatory Affairs. “There’s a lot of great contractors out there, but they have to understand and respect that there are certain requirements in health care dictated by codes and standards that they are probably not used to. Especially when it comes to the [National Fire Protection Association’s] Life Safety Code®. For example, they may take a shortcut and unknowingly compromise fire barriers and smoke compartments that put lives at risk.”
Hiring contractors who specialize and are trained in health care construction can streamline projects, better maintain regulatory compliance during a PDC project and — most importantly — better protect patients. Mark Howell, a Seattle-based senior vice president at construction company Skanska, says it is paramount that construction staff understand they are entering a highly sensitive, sterile environment.
“When tradesmen have that training, they understand all those nuances within a hospital. They know you can’t just go into a hospital and start shutting down systems to work on them because of the impact on life safety requirements and the ability to operate the hospital,” Howell says. “It’s about understanding you need to work with the facilities team and learn their shutdown processes and their tie-in processes for utility work; understanding infection control requirements and following ICRA; and asking, ‘Are all of our barriers and negative pressures in place?’ Creating that clean environment and keeping the construction on one side of the barrier. It’s such a unique facility because not only is a hospital 24/7, but it also is caring for people’s lives and loved ones.”
There is a big difference between being compliant with health care construction building codes and meeting regulatory requirements for the provision of health care — which, for example, mitigate waterborne pathogens and health care-associated infections and include maintaining proper temperature, humidity, and positive and negative air pressure, says Dennis Ford, MHA, CHFM, CHC, FASHE, director of corporate facilities management support at Atrium Health and ASHE president-elect.
For example, Ford once had to shut down a hospital construction project because, despite promises to minimize their environmental impact, the noise and vibration from contractors were adversely impacting the nearby neonatal intensive care unit and putting premature babies at risk. At another jobsite, Ford once caught contractors crawling inside the air ductwork to speed up the installation — blatantly violating infection prevention policies.
Because health care organizations are responsible for the safety and well-being of all patients at all times, it is imperative that all contractors follow an organization’s clean construction protocols, policies and procedures — and that facilities managers ensure that compliance is met, Beebe says.
Visit ASHE online to learn more about its certification programs.
Chris Dimick is content development and communications manager at the American Society for Health Care Engineering and production editor of Health Facilities Management (HFM) magazine, and Jamie Morgan is senior editor of HFM.