Engineers search for savings in Energy Star Treasure Hunt
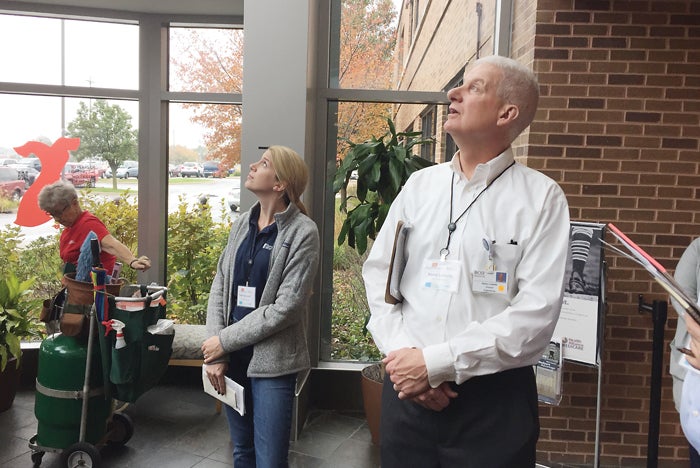
Lots of Light: Paige Engelhardt, an engineer at Farnsworth Group, and Kerry Loiselle, director of engineering for OSF HealthCare St. Joseph Medical Center, discuss the efficiency of the many windows in the lobby of the hospital.
Photo by Ed Avis
OSF HealthCare St. Joseph Medical Center in Bloomington, Ill., discovered $206,872 in treasure in early November. No, the hospital didn’t dig up a long-lost cash box buried in the basement. Rather, a team of facilities personnel conducted an Energy Star Treasure Hunt that uncovered potential energy savings equaling that amount.
It was the first-ever Energy Star Treasure Hunt conducted in a hospital. I was asked by the American Society for Healthcare Engineering to document the event, and decided that the best way to do that was to jump in and join the group on this quest.
Team-based approach
Energy Star Treasure Hunts date to 2014, when the Environmental Protection Agency (EPA) released a guidebook based on the experience of Toyota and other industrial Energy Star Partners who pioneered the concept of a focused, team-based approach to finding potential energy savings in a facility. The events typically take two or three days; the first or second day is the actual hunt, and the final day is the reporting.
Resources
The EPA published a 34-page PDF about how to organize a treasure hunt — including checklists, calculators and other handy tools — after learning how effective they were in identifying energy-saving opportunities and empowering employees to implement the solutions, explained Clark Reed, the EPA national program manager of Energy Star commercial buildings, who participated in the event.
The event at OSF St. Joseph, part of OSF HealthCare in Peoria, Ill., was held Nov. 2-3. The potential savings found during those days reveal how valuable the process could be to any hospital.
“It would take us a million dollars in revenue to earn an equivalent amount of profit,” noted Paul Pedersen, M.D., the hospital’s chief medical officer, who attended the closing-out report at the end of the second day. “Job well done.”
Meeting the experts
I arrived at OSF St. Joseph at 7 a.m. on the first day, and discussions with the other attendees during the first 30 minutes or so revealed that I was among a group of facilities and energy experts, ranging from the EPA’s Reed to Ray Curry and Don Mulch, front-line facilities operations managers at the hospital.
A number of participants came from outside the hospital. For example, pharmaceutical firm Bristol-Myers Squibb provided two sustainability experts — Zach Newman and Bill Perhacs — who had conducted Energy Star Treasure Hunts at nine of their company’s facilities around the world. Their expertise proved pivotal in our hunt. Another essential pair were Chad Whitehead and Steve Smith, contractors for the local electricity supplier Ameren Corp., who made sure we recognized potential electricity saving opportunities and the rebates associated with many of them.
Advice on hunting for energy savings
- The team should include experts from various disciplines, including engineers, facility experts and electrical specialists as well as vendor representatives and members of various hospital departments. Everyone’s expertise, either about the local situation or about energy saving in general, contributes to the success of the event.
- It pays for the potential leader of the event to have participated in a Treasure Hunt in another facility before leading one.
- The reporting-out event should be directed at key leaders in the hospital so that they understand the possibilities, and all team members from the hospital itself should participate in the report-out so that they get some face time with leaders.
- Remember that dollars speak. Quantify the potential savings areas as thoroughly as possible.
We received a background briefing from Patrick Costello, manager of energy and sustainability for OSF HealthCare. Costello explained that we would be divided into two teams to investigate different portions of the facility during most of the first day, and then come together to compare notes and calculate potential savings.
Then Kerry Loiselle, the facility’s director of engineering, gave us the lay of the land: The main part of the facility was built in 1967, and additions have grown its footprint ever since. Today, the campus includes that main hospital building, two stand-alone physician office buildings added in the late 1980s and early 1990s, a surgery unit added in 1998, the Center for Advanced Medicine built in 2004, an obstetrics addition built in 2011, and various smaller structures, totaling approximately 550,000 square feet.
Loiselle explained that some parts of the campus are united by building automation systems (BAS), while other parts have stand-alone BAS of varying ages. Similarly, some parts of the campus use the central boiler system — parts of which are original to the 1967 construction — while others use stand-alone units that were added more recently.
“As with any hospital, you start with one building and add on as you need to,” Loiselle said. “We have a master plan, but when you start adding on, you can get locked in by the older buildings. It’s a challenge.”
Before dividing into teams, Costello and Loiselle gave a safety briefing and handed out earplugs to use in the boiler rooms.
Costello aimed to put representatives from each discipline on each team. I was assigned to Team 1 with Loiselle, Mulch, Newman, Smith, Paige Engelhardt [an engineer at Farnsworth Group, a firm that consults with OSF Healthcare], and Octavian Dumitrescu, director of facilities management at two other OSF HealthCare facilities in Illinois.
Into the hunt
My team went straight to the hospital’s main boiler plant, which is more than 50 years old. The engineers in our group immediately started asking pertinent questions: How much steam is produced? Is the flow constant? Does it vary with the seasons? Who are the users?
Loiselle and Mulch answered those questions, and explained that the need for steam does not go away in the summer, as certain parts of the hospital, like the sterilization department, need steam year-round.
Newman observed that steam was flowing steadily from the bottom of one of the boilers, a sign of a potential problem with the steam trap. He also noticed that a water-cooled compressor was not operating as expected, possibly indicating a defective solenoid valve.
“Right now, I’m just looking for things that don’t look right,” Newman said.
We exited the boiler room through a tunnel to the main hospital. Even there, the experts sniffed out savings, in this case the inefficient fluorescent bulbs in the ceiling panels. Mulch explained that the old bulbs are being replaced with LED lights as they burn out.
The conversation flowed to lighting in general. Ameren’s Smith mentioned that some of the hospital’s exit signs were not LED, and that the utility offers a $20 rebate on every newly installed LED exit sign. Newman brought up the idea of motion sensors to turn off lights in unoccupied spaces, but warned that they shouldn’t be used in certain spaces like boiler rooms where workers might be toiling out of sight of the motion sensor and become trapped when the lights suddenly go out. Instead, he recommended putting the lights on timers so that 10 minutes before shut-off, the lights flash, alerting anyone who is still in the room.
We next visited one of the campus’ air-handler rooms. Overall, the air-handler rooms were clean and presented few energy-saving opportunities. However, the question of temperature and airflow setbacks came up regularly during these stops. For example, Loiselle was asked if the temperature in the administrative spaces could be set back in the evenings. Perhaps, he said, but unfortunately the same air handler also supplies one of the lobbies, which could complicate the setback.
In one of the air-handler rooms, Engelhardt noticed that air was leaking out of one of the ducts, indicating a seal in need of repair. Similar situations were spotted in other locations.
We had to don surgical gowns, hats and booties for our team’s last stop: one of the hospital’s operating suites. Naturally, the consideration of saving energy in an operating suite takes a back seat to the need to have that room available 24/7 on a moment’s notice. Nevertheless, the team wondered about turning off the lights when the room was not in use and, perhaps, reducing the number of air exchanges.
During our tour, we also observed some of the hospital’s existing energy-saving devices. For example, beside one of the rooftop air handlers, we inspected a heat-recovery unit. When air flows over the coils in the unit, it heats or cools the liquid in the coils, which then flows to another part of the air handler where it preheats or cools the air coming from the outside.
Additionally, an important part of the hunt is looking for safety hazards. For instance, we encountered several spots where pipes or other structures hung low enough that workers could hit their heads.
Adding it all up
The teams reunited in the meeting room in early afternoon and gathered around flip charts to debrief. At this stage, we were encouraged to write down all possible savings opportunities; calculations and feasibility would come later.
Among the ideas from my team were fixing the broken solenoid valve on the water-cooled compressor; setting back the temperature in various spaces; conducting a steam-trap survey; replacing the old light bulbs; and half a dozen others.
One idea that we added that was not the result of direct observation was suspending irrigation of the landscaping. Dumitrescu explained that he had done that at one of the hospitals he oversees, and the savings were significant.
“The city even came out to the hospital and told us they thought our water meter was broken,” Dumitrescu said. “I said, ‘No, we just stopped watering the grass.’”
Team 2, which had toured the chiller room and several other areas not seen by Team 1, suggested replacing damaged or missing insulation on various lines; replacing a number of older motors they had discovered during the tour and adding variable-frequency drives (VFDs) to them; valving off unit heaters that are connected to the steam lines all year; and upgrading the BAS in certain spaces, among others.
Each item on the flip charts represented an energy-saving opportunity, but we didn’t have time to evaluate each one, so the teams were told to select four or five of their best and calculate the potential savings. There were some duplicates, so the teams negotiated to make sure no opportunities were investigated twice.
A small group of participants went back into the spaces to perform follow-up research on some of the opportunities, and to photograph the priority areas.
Team 1 looked into replacing the old lights with LED lamps; replacing the older, inefficient motors; reducing the number of air exchanges in the operating room when it’s not in use; and developing a setback for the exhaust fan in the kitchen.
I was tasked with determining the potential savings from replacing the motors and adding the VFDs. First, I priced out new motors of the appropriate horsepower and VFDs for those motors, and then calculated the potential energy savings using online calculators that do just that.
For example, to determine the potential savings from adding a VFD to a motor, a calculator on the website for motor manufacturer WEG Electric Corp., Duluth, Ga., asks that you enter the horsepower of the motor, its application, its efficiency rating, the cost per kilowatt-hour, the cost of the VFD, and the flow rate and daily hours of operation. When I entered those data for the motor I was evaluating, the calculator computed the hospital’s savings as $2,955 per year.
By adding in the savings from the high-efficiency motor compared with the current, standard motor, and the rebate Ameren offers for installing the VFD, and then subtracting the cost of the motor and the VFD, I calculated that the change would provide $1,468 in savings the first year. I extrapolated that figure to all of the other motors that needed to be replaced, and determined that the hospital could save more than $7,000 in the first year and more than $16,000 in subsequent years. The payback period for the switch was calculated at 0.57 years.
These figures, plus similar calculations for all of the other opportunities identified, were summarized on PowerPoint slides. The totals were impressive: We quantified nine opportunities that totaled $206,872, and noted 18 others that we did not have time to quantify.
The second day of the Treasure Hunt was spent going over our presentation, ironing out a few remaining questions and rehearsing.
By mid-morning, Pedersen joined the group, and several other key people called in via WebEx. Loiselle led the report-out and explained the potential savings of each opportunity the teams had discovered.
Naturally, with more than $200,000 in potential savings identified, the leaders attending the event were impressed.
“The group did a great job identifying and quantifying the potential energy-saving opportunities,” Costello said. “This was a truly successful event.”
Spreading the idea
The savings opportunities we identified during these two days fall into several categories: Some are quick fixes, such as resealing leaky ducts; and others are long-term projects that require capital investment, such as replacing the old lighting and motors.
“In our experience at Bristol-Myers Squibb, at least half of the identified projects get done,” Newman said.
According to the EPA Treasure Hunt guide, the next step is for facilities leaders to further refine the recommendations and report again in 30 days about the priorities and the strategy for implementing the recommendations.
In the bigger picture, the EPA hopes that the concept of Energy Star Treasure Hunts in hospitals catches on. The EPA’s Reed, who filmed the event, said his hope is to spread the idea throughout the health care field.
Ed Avis is a freelance writer based in Chicago.




