Results of the 2024 Hospital Operations Survey
Image from Getty Images
Hospital maintenance is a demanding job, but it’s a job made even more challenging for facilities managers who see to the heightened needs of older buildings. It takes significant capital expenditures to maintain building systems that are either reaching the end of their lives or are no longer compatible with modern technology or safety requirements. And keeping these buildings operating without impacting patient care demands a full range of specialized skills.
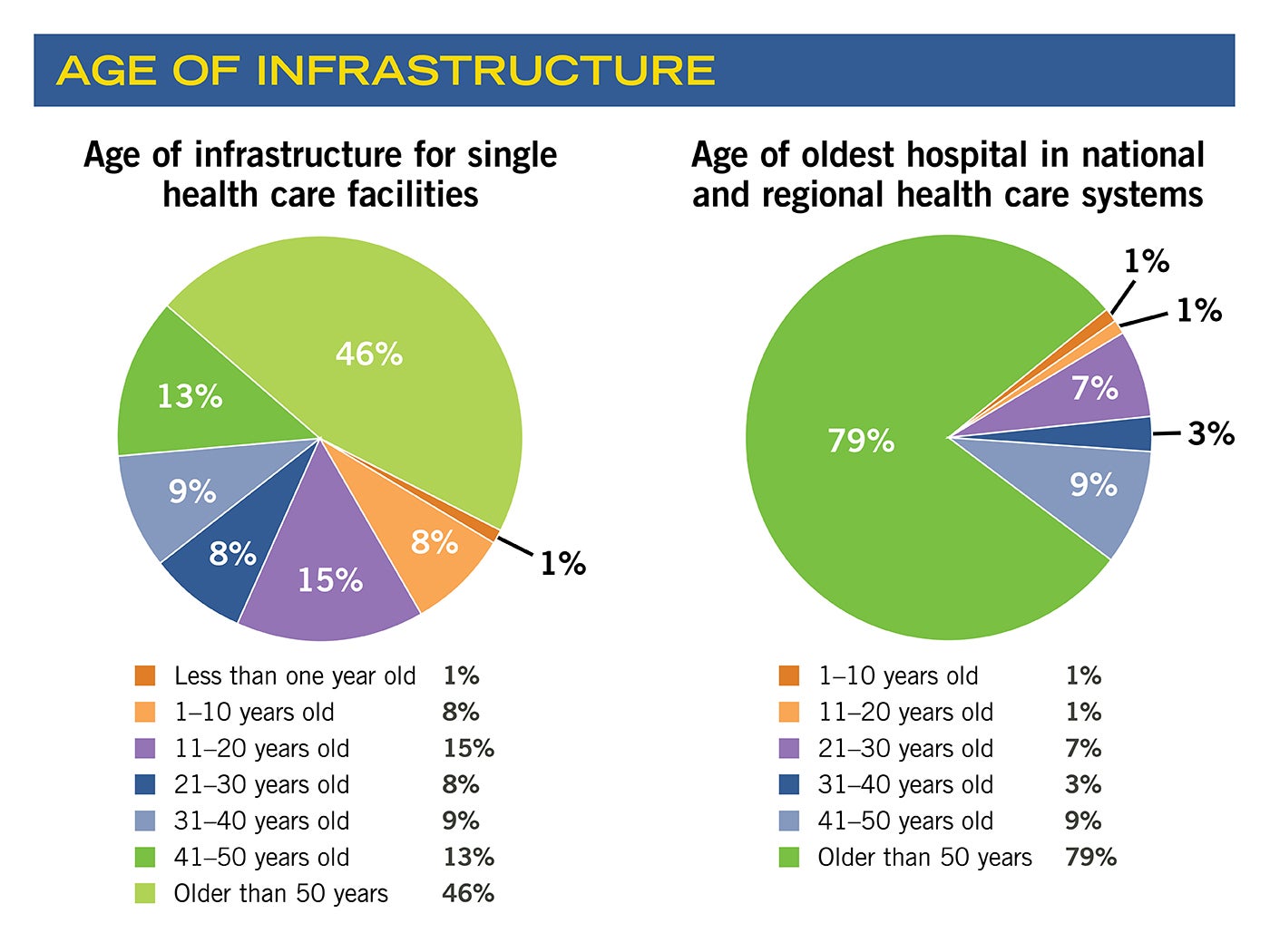
With well over half of the more than 430 hospital and health system facilities managers and executives surveyed for the 2024 American Society for Health Care Engineering (ASHE) Hospital Operations Survey overseeing at least one facility that is more than 50 years old, it’s perhaps no surprise that aging infrastructure tops their list of challenges. A full 80% of survey respondents cite aging facilities and infrastructure as their leading concern, and another 58% point to lack of funding and staff recruitment and retention as their No. 2 challenge.
Fortunately, respondents to the inaugural Hospital Operations Survey, conducted by ASHE’s Health Facilities Management magazine, also shared the creative solutions they’re developing to maintain their intensive environments with the resources available.
Solution prioritization
Without the right team or appropriate resources to support older buildings, maintenance needs build up. As a result, “Deferred maintenance is a huge problem,” according to Chad Beebe, AIA, CHFM, CFPS, CBO, FASHE, deputy executive director for ASHE Regulatory Affairs. “The last time we looked, there was more than $390 billion worth of deferred maintenance out there not being done in health care facilities collectively across the United States,” he continues, citing a 2021 ASHE study of deferred infrastructure maintenance across the nation’s health care facilities.
As facilities managers well know, deferred maintenance left unattended turns minor issues into major system failures.
“Probably the best example of this are roofs,” says Jonathan Flannery, MHSA, CHFM, FASHE, FACHE, senior associate director for ASHE Regulatory Affairs. “A roof leak can be an annoyance, but it’s not a big deal to repair. The issue is that recurring roof leaks are a sign of the beginning of the end of the life of the roof. If that’s not addressed in a timely manner, the entire system can fail.”
Effective management of deferred maintenance typically relies on two factors: funding and staffing. As respondents to the survey revealed, neither of these factors are keeping pace with deferred maintenance needs. Less than half of all deferred maintenance funding requests were funded for 79% of survey respondents, with 43% receiving 10% or less of their requested funding. And while 64% of respondents say their staffing needs over the last three years have increased, only 27% have seen actual increases in maintenance staffing numbers.
As one survey respondent shares, “Budget restrictions have limited equipment upgrades and replacements, creating more equipment failures that require more labor.”
Respondents whose staffing needs have increased while actual staffing has decreased attributed this understaffing to budget cuts (66%) and staff resignations (52%) and retirements (45%) left unfilled.
“It’s hard enough to get funding for capital improvements. We just try to prioritize the best we can,” says one survey respondent.
This prioritization is key because despite the hurdles respondents report facing, they are moving forward with new solutions for recruiting staff, securing funds and effectively managing maintenance loads.
Data tells a story
Brady Housden, CHFM, CHC, facilities project manager at Community Health Network in Indianapolis, has been among those professionals who have received only partial funding for deferred maintenance requests. While with another health system, Housden found that successful requests were generally backed up by a story connecting maintenance funding to patient care. “We would connect why we need the money to fix one thing to the short- and long-term effects of not doing that thing,” he says.
For 64% of survey respondents, explaining to executive leadership how infrastructure impacts patient care is the most effective strategy for securing deferred maintenance funds. Fifty-nine percent report that tying upgrades to regulatory compliance also makes a compelling case. This approach often depends upon having data to build a case.
“Obtaining capital funding for facilities budgeting from the [executive leadership] and creating a solid fact-based business case is where a lot of facilities directors need support,” says Michele Mucia, director of health care strategy with Nuvolo, an international provider of facility assessments and computerized maintenance management system (CMMS) program development. “You have to know the equipment deficiency priority level based on code and compliance metrics first.”
Mucia adds that she is often asked by facilities managers how they can build the case for prioritizing investment in building equipment over medical equipment. The answer, she says, comes down to facility condition assessment capital planning data that demonstrates the risk of inaction versus action.
“You must tell the financial story of how [the system] can benefit from reviewing historical equipment spending work orders, calculating demand flow on antiquated equipment, measuring full-time equivalent (FTE) employee costs, renegotiating vendor contracts and obtaining proper repair and replacement proposals from original equipment manufacturers,” she says.
Most survey respondents (72%) report that they are tracking and benchmarking their maintenance activities, such as work order completion rates, making it easier to pull historic maintenance data that can support future funding requests. In addition, 80% of survey respondents have adopted CMMSs that provide the data for effective storytelling.
“Work order and preventive maintenance counts, completion rates, time to close and forecasted preventive maintenance all help with scheduling staff and following up on teams that need additional support or resources,” says one survey respondent. Respondents advise tracking equipment failure rates, unscheduled downtime of critical infrastructure, patient room closures for maintenance and daily work order percentage completion.
“Tracking equipment failures and downtime has led to better root-cause analysis and aided in acquiring additional capital funds,” shares one professional.
To maximize business cases, Mucia suggests ensuring tools, such as a CMMS, are standardized across locations.
Transition to RCM
Many facilities managers are working to get ahead of maintenance activities by adopting maintenance strategies that have proven effective in maintaining complex equipment across other industries. Reliability-centered maintenance (RCM) is increasingly being used by health systems — and 21% of survey respondents — to apply the most appropriate maintenance methods and schedules to specific assets.
Unlike a strictly preventive maintenance strategy, RCM might dictate that reactive maintenance is suitable for replacing air-handling unit filters, whereas a predictive maintenance approach is essential for preventing air-handling unit failure. The key to this approach is understanding the causes and effects of failure for each individual asset.
“There’s a bunch of different ways to get started, but it’s a complete mindset shift to how we’ve been doing it,” Housden shares. It’s why Housden hired a champion to lead the RCM effort at his organization. He adds, “It’s a multiyear effort to switch over.”
Beebe agrees, noting, “It’s going to be an uphill lift, changing the way we take care of our assets. A complete culture shift needs to happen.” He adds, “In the long run, it will make sure that you’re using your FTEs as efficiently as possible. It allows them to focus on priority work and will help with compliance by ensuring that critical items are getting the attention they need and that noncritical items are not distracting from the mission.”
ASHE is developing tools to support this shift by helping facilities managers secure buy-in from leadership and get a commitment to provide resources necessary to enable the shift to RCM.
“These resources will help professionals better tell the story of maintenance needs before they become a problem and need to be put on the deferred maintenance list,” Beebe says.
Like Housden, other professionals have created dedicated positions to begin implementing RCM techniques and build awareness of the strategy’s value.
Through asset life cycle management, organizations are incorporating RCM techniques, including preventive maintenance procedures and proactive equipment condition evaluations. Survey respondents are adopting technology capable of detecting the earliest indications of equipment degradation, including vibration and oil analysis, infrared and ultrasound testing, and monitoring-based commissioning.
“We are in the infancy of this process after a culture of run-to-fail,” shares one survey respondent. “This [shift] has helped leadership understand the impacts of equipment failure … Failures are tracked in the CMMS and tied to repair costs. We evaluate all capital replacements using the [National Fire Protection Association’s NFPA 99, Health Care Facilities Code] risk assessment table to help leadership understand total risk likelihood and consequence.”
Benchmarking staffing needs
Process changes have helped health care facilities improve management of infrastructure, but because many report being understaffed, organizations are being challenged to optimize allocation of FTEs. Many of the respondents note that better data on staffing needs is crucial.
Housden is among the 47% of survey respondents who perform staff benchmarking, and of that group, he is also part of the 46% who use industry data to guide their benchmarking standards. For Housden, those resources include the International Facility Management Association’s (IFMA’s) North America Operations and Maintenance Benchmarking Report and the Benchmarking 2.0: Health Care Facility Management Report, released by ASHE, IFMA and the Canadian Healthcare Engineering Society.
At Housden’s facility, staff was added to maintain additional square footage, but roles also shifted to meet the most pressing needs. “There was internal movement as we dialed in what we use our available FTEs for. We eliminated some management and supervisory roles when people left or retired and turned those into more operational roles.”
Fifty percent of respondents that perform staff benchmarking are doing so using internal data, gathered from maintenance activity tracking. Benchmarking can be a valuable way to understand staffing needs and better allocate resources. Yet 19% of survey respondents report being unsure whether their organization performs staff benchmarking. Without this data-backed understanding of staffing needs, it will be difficult for facilities professionals to advocate for more staff. It may also cost departments that are contracting out services more money on tasks that could be performed in-house.
As one survey respondent reports, “[Benchmarking] has helped us realize costs for contracted services and showed a need for training to self-perform some of the contracted services to save costs.”
Outsourcing fills gaps
Survey respondents report contracting out 33% of facilities maintenance activities on average. Many of these are activities that have traditionally been recommended for outsourcing to specialized partners, such as fire alarm inspection (85%) and elevator maintenance (82%).
However, the survey also revealed that outsourcing is addressing gaps in staffing where it has become more difficult for health care organizations to deliver competitive wages for in-demand specialists. For example, 73% of survey respondents report a gap in staffing for heating, ventilating and air-conditioning (HVAC) and controls technicians, and 62% are contracting this work out.
“I’m surprised that’s No. 1,” Flannery says. “If you’re doing HVAC construction or service work, you don’t know if you’re going to have another job after you’re done with the current job being worked on. The health care field offers an 8-to-5 job at a facility. You get stability, you get vacation time. The security health care offers is significantly greater than what is normal in the field. We may not pay as much, but the benefits and stability have always seemed to override that.”
Housden says that’s no longer the case. “We just can’t compete wage-wise. An HVAC company is going to pay them a lot more,” Housden says. With 61% of survey respondents agreeing that higher starting compensation is the most effective recruitment tool, this inability to keep pace presents a challenge.
This has added to a seemingly never-ending cycle, Flannery says, since contracting out this work typically increases maintenance costs. What’s more, it can create inefficiencies in workflow. “When you have a hired staff member, you have a relationship,” Flannery explains. “With a third-party contractor, they send whoever they have available now. Then you’ll need to explain the issue and what you need all over again.”
But facilities managers are not giving up on building internal staff, both in numbers and skills. Twenty-seven percent of survey respondents have improved their interview processes and participated in job fairs to find and hire qualified staff.
Once staff is recruited, 37% report ensuring career growth pathways and paying for employees’ continuing education opportunities to help retain that staff and ensure proper care of the physical environment.
RELATED ARTICLE: Managers look outside to build recruitment pipeline
Recruitment challenges are not new to health care facilities managers. However, more of these professionals are deploying creative strategies to create a pipeline of talented professionals to keep pace with staffing needs.
For Brady Housden, facilities project manager at Community Health Network in Indianapolis, that means looking beyond the health care field and finding necessary skill sets from operators within other critical environments.
“We went after people from data centers who are used to having to keep critical equipment running 24/7. Those skills translate over, especially to higher-level health care maintenance positions,” he says. “For entry-level maintenance or facilities people, we just required a year of some sort of construction or maintenance experience so that they had some of that basic knowledge. Then we provide a lot of the training on working in a hospital. Even for professionals from other critical environments, health care is a whole other animal.”
Housden is also working to partner with local high schools to shape internships that introduce students to the facilities world.
“It’s key to get young people into the system and make sure there’s opportunities for everyone to engage,” he says. Nineteen percent of respondents to the 2024 Hospital Operations Survey, conducted by the American Society for Health Care Engineering’s (ASHE’s) Health Facilities Management magazine, agree that an internal apprenticeship or internship program can be an impactful recruitment strategy.
As employees with little health care experience come on board, in-house development becomes essential.
“We have developed a pretty extensive training program to train someone with a very basic level of experience on how to work in a hospital,” Housden shares. “This includes what to look for with dust control, infection prevention and noise — all the way to customer service.”
It’s that last piece that may be the most compelling for new recruits. Customer service, Housden explains, is all about “how to deal with people who are at the highest point of their lives, welcoming a new family member; to the lowest point, who are saying goodbye to somebody.”
It’s all about connecting facilities maintenance to patient impact.
When it comes to retention, compensation is key for 48% of Hospital Operations Survey respondents, and 37% of respondents emphasize the importance of ensuring a strong career growth pathway.
To help create this path forward, ASHE offers a monograph to help health care facilities managers conduct effective succession planning for their departments and individuals in all positions to develop a path for personal career development. “Succession Planning: Preparing for the Future of Your Facility and Career” shares strategies for providing employees with the support and resources needed to fuel their career growth.
Megan Headley is a freelance writer based in Fredericksburg, Va., and Jamie Morgan is senior editor of Health Facilities Management.