The road to sustainability can get bumpy, survey finds
 Buying decisions based on initial costs, apprehension over performance of new technology and a perception of "green washing" in the marketplace commonly prevent health care facility professionals from buying or specifying products that could make their hospitals more sustainable or energy-efficient.
Buying decisions based on initial costs, apprehension over performance of new technology and a perception of "green washing" in the marketplace commonly prevent health care facility professionals from buying or specifying products that could make their hospitals more sustainable or energy-efficient.
Those are key among interrelated actions and perceptions that are preventing health care facility professionals from taking actions to increase levels of sustainability and energy efficiency in hospitals, according to a recently released survey.
The survey was conducted as part of the "Economics, Efficiency, Energy & Environment: Making the 4Es Work Together in Healthcare" seminar series conducted by the Corporate Realty, Design & Management Institute in partnership with the Health Care Institute of the International Facility Management Association (IFMA). The two organizations presented the seminars in 20 U.S. cities in 2010-2011.
The 1,251 respondents included architects, designers, engineers, hospital facility managers, health care engineers, project managers and contractors who are either employed by a hospital or are contracted to do work for them.
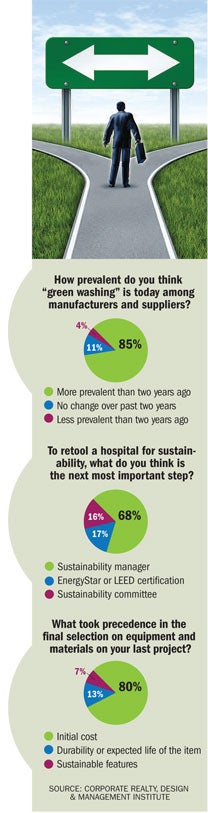
Buying products and services based on first cost continues to be the industry norm, with 80 percent of the respondents citing that is how they select equipment and materials, says B. Alan Whitson, board of advisors, IFMA Health Care Institute, and president of Corporate Realty, Design & Management Institute.
"If you look at the whole host of things that go into buildings — you see it everywhere, from lamps to floor coverings to concrete to types of construction methodology — the industry has a tendency to base everything on first cost," says Whitson. "It may not necessarily be the best product or the best service or the best way of doing things."
The barriers to buying based on lifecycle costs is illustrated by a basic example in the choice between buying a PAR 38 halogen lamp that will cost about $6 or a PAR 38 LED lamp that costs $55. "Most facility managers won't get past the first part of the conversation. They'll be told 'we can't afford it,'" says
Whitson. The halogen lamp uses 79 watts, lasts about 5,000 hours and will need replacement nine times over 10 years of use. In comparison, the LED uses 17 watts and lasts about 45,000 hours over 10 years, says Whitson. The result? The halogen has a 10-year life-cycle cost of $377 compared with the LED's $109, he explains.
A major part of the obstacle to increased sustainability and efficiency is the inability of industry professionals to prepare and communicate lifecycle cost analysis effectively to C-suite executives, says Glenn Fischer, vice president, IFMA Health Care Institute, and executive vice president of Corporate Realty, Design & Management Institute.
The failure to install equipment, systems and materials that save energy is a missed opportunity, says Whitson. If a hospital operates on a 4 percent total margin, saving $1 in energy costs equals $25 in revenue. For the average-sized hospital with 200 beds, that's the equivalent of an additional $7.2 million in revenue.
Nearly 80 percent of respondents cited concerns that new energy-saving technology will not deliver projected performance as a reason for not buying or specifying it. Similarly, 85 percent of respondents say that green washing is more prevalent than two years ago.
Whitson says overcoming these barriers to increased sustainability and energy efficiency in health care facilities may require better education by manufacturers about their new technology.
In terms of the next step in making a hospital more sustainable, 68 percent say that appointing a sustainability manager is most important, followed by 17 percent who say achieving an Energy Star rating or LEED certification. The survey found that 16 percent call establishing a sustainability committee the next most important step.




