Going Greener
Hospitals plan to make their facilities greener, knowing that it is one way to cut or at least control costs and improve the indoor environment for staff and patients. But hospitals frequently must limit their sustainability actions because of ongoing financial challenges, including the prospect of reduced reimbursements under health care reform.
Nevertheless, the Energy Efficiency Indicator (EEI) survey conducted earlier this year by the American Society for Healthcare Engineering (ASHE), the Johnson Controls Institute for Building Efficiency and the International Facility Management Association, found that 66 percent of the health care respondents
are paying more attention to energy efficiency than they were a year ago.
 Robin Guenther, FAIA, LEED AP, sustainable health care design leader at architectural design firm Perkins+Will, New York, says more hospitals will continue to move forward with making their facilities sustainable for a variety of reasons, even if the investments are modest for now.
Robin Guenther, FAIA, LEED AP, sustainable health care design leader at architectural design firm Perkins+Will, New York, says more hospitals will continue to move forward with making their facilities sustainable for a variety of reasons, even if the investments are modest for now.
First, the launch of the U.S. Green Building Council's LEED for Healthcare rating system is likely to produce increased interest in sustainable building, she says. Second, the increased recognition of health care facilities that are champions of green operation initiatives also is generating greater interest in
sustainability.
In addition, the health care sector is "paralleling larger market movement toward sustainable practices" in such areas as healthier materials and chemicals avoidance, healthy food, green cleaning and green building, she says. Plus, it's good business to be green.
"As the business case for these practices continues to yield economic benefits, hospitals will continue to implement programs," Guenther says. "Finally, organizations that are undertaking these initiatives are finding they support broader organizational transformation and support staff retention and satisfaction."
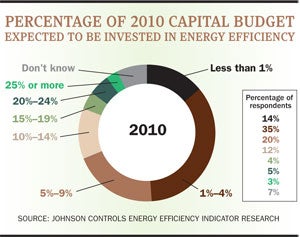
How much hospitals spend on energy efficiency — a key component of sustainability — is another matter. The EEI survey says that half of the hospitals that responded lack a capital budget to make energy-efficiency investments. Even though 68 percent of the health care respondents said they expect to invest in energy-efficient capital equipment in the next 12 months, 49 percent said the amount invested would be 4 percent or less of the capital budget, according to the EEI survey.
Cost savings is king
That being said, it's no surprise cost savings is the primary motive for energy efficiency investments by health care facilities. In fact, 88 percent of the health care organizations that responded to the EEI survey said cost savings is very or extremely important and 99 percent of the organizations said it is at least somewhat important.
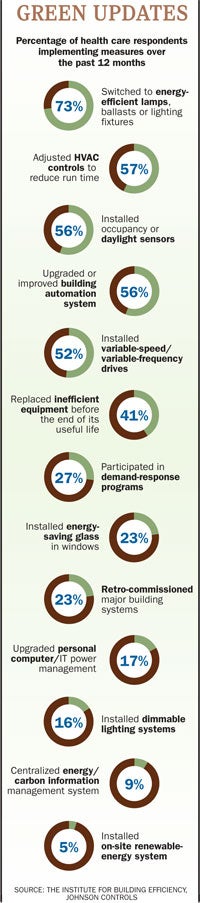
The survey reports that the most common energy-saving actions hospitals take are retrofitting to energy-saving lighting and adjusting HVAC controls schedules,
followed by installing in-occupancy sensors and new DDC controls. All are fundamental steps, but still energy savers, says Derek Supple, program director for global energy and sustainability, Johnson Controls.
The results of the ASHE/Association for the Healthcare Environment (AHE, formerly the American Society for Healthcare Environmental Services) 2010 Health Care Facilities Sustainable Operations survey conducted with Health Facilities Management earlier this year are similar to EEI's findings. Our survey data found the most common energy management initiatives hospitals undertook the last two years were implementing a preventive-maintenance plan, retrofitting to energy-efficient lamps and installing occupancy sensors or timers.
One noteworthy trend that emerged from the EEI survey shows that 27 percent of hospitals utilize a demand-response system with their local utility to save energy during summer peak loads, says Supple. Demand response involves the utility sending a signal or message to the hospital to take actions to cut their power usage to reduce energy consumption. A few basic steps include adjusting HVAC set points, dimming lights, reducing power to noncritical computer servers or putting computers in standby mode, says Supple.
Rick Smith, director, energy solutions, Johnson Controls, foresees another possible trend for hospitals in which the piecemeal approach to energy efficiency gives way to a more sophisticated building strategy to maximize energy savings. "I think the consideration of a holistic approach versus a one-off improvement will perhaps get more attention as we go down the path here," he says.
"If we reduce the electrical load, we reduce the heat load, which means we're going to have a different-sized application, perhaps, for our central chiller or chilled water system," Smith says. "So, if we take all those interactions into play as one large system versus individual retrofits, you'll have first-cost reduction, you'll have life-recycle improvement for the equipment, and you'll have a larger energy savings gain."
Waste not, want not
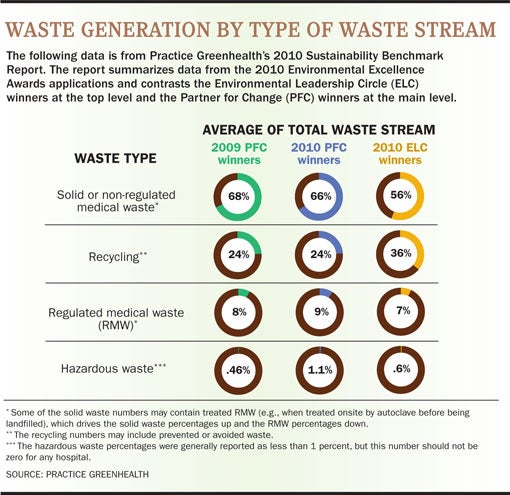
Hospitals generate nearly 6 million tons of garbage annually, and that's not counting recycled waste, according to a recent report using data from Practice Greenhealth. It's little wonder that finding ways to reduce the waste stream is becoming a higher priority and that recycling only will become a bigger imperative, along with boosting energy efficiency, experts say.
"Hospitals seem to have success in waste reduction and energy efficiency for two reasons," Guenther says. "First, both these programs can yield substantial economic savings. A dollar saved in operations is a dollar transferred to the bottom line.
"Many hospitals have funded their sustainability coordinators from their savings in waste fees alone, largely through reducing overall volume as well as the volume of regulated medical waste. Secondly, both energy and waste appear to have economical 'low-hanging fruit' strategies," she says.
Because regulated or hazardous medical waste is much more expensive to dispose of than nonregulated medical waste, it pays to ensure waste streams are separated correctly. Recycled waste usually is hauled away for no charge or the hospital may get a rebate depending on the agreement with their waste hauler, sources say.
 "Therefore, if you move material from a more expensive waste stream to a less expensive stream, you will ultimately save money," says Dr. Linda Lee, health care solutions operations director, Waste Management Inc., Houston.
"Therefore, if you move material from a more expensive waste stream to a less expensive stream, you will ultimately save money," says Dr. Linda Lee, health care solutions operations director, Waste Management Inc., Houston.
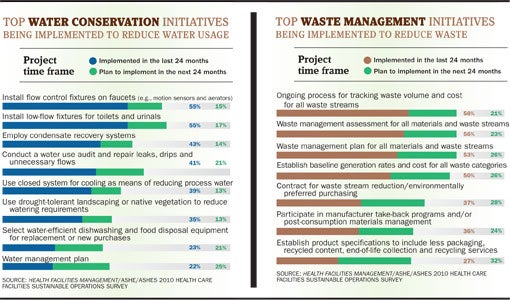
The financial advantages of smart waste disposal are causing more hospitals to establish plans. The ASHE/AHE/HFM survey found that the top three waste management initiatives hospitals implemented within the past two years were to track waste volume and waste stream costs (58 percent), develop a waste management assessment for all materials and waste streams (56 percent), and to establish a waste management plan (53 percent). The trend shows continued growth in those waste-reduction strategies.
"As we can find opportunities to move material into more beneficial use rather than just throwing it away, we're seeing a high level of engagement from hospitals," says Lee. "Hospitals want it to be cost neutral or they don't want to spend any more money on waste disposal than necessary."
Many hospitals can save hundreds of thousands of dollars on waste disposal just by learning how to handle their waste stream properly, says Lin Hill, Environmental Excellence Awards program manager, Practice Greenhealth.
The new oil
Some sustainability experts are calling water the new oil. Certainly, in areas of the Southwest and West water already is a precious commodity. But despite its scarcity in some regions, water conservation is not an area that all hospitals emphasize in their sustainability efforts.
The ASHES/AHE/HFM survey found that only 41 percent of health care facilities measure their water savings. In comparison, 69 percent measure their energy savings and 61 percent measure their waste reduction savings.
Despite the lower number, Melissa Cain, regional manager, Phigenics, a water-management consulting firm based in Naperville, Ill., says the trend is for hospitals to expand their water conservation efforts. "I would say that over the last five years of working with our health care clients that water conservation is a priority. If it's a facility that's already addressing sustainability, water is a big part of that," says Cain.
The ASHE/AHE/HFM survey shows the most commonly implemented water saving initiatives are installing such control fixtures as motion sensors or aerators on faucets, installing low-flow fixtures on toilets and urinals, and employing condensate recovery systems.
Efforts to reduce process water typically vary by region, says Guenther. "In terms of process water use, more hospitals in arid regions are planting drought-resistant vegetation and using captured condensate for cooling towers, and captured rainwater or condensate for drip irrigation, but have been challenged to make the business case for installation of cisterns," she says. "Few are implementing grey-water or black-water systems due to continued concerns about regulatory barriers and infection control."
A major water guzzler at hospitals is landscaping, says Winston Huff, CPD, LEED AP, project manager/sustainable coordinator, Smith Seckman Reid Inc., Nashville, Tenn. "The largest irrigated crop in the U.S. is turf grass and at some hospitals up to one-third of their water usage can go into watering the grass," he says.
Huff says there is a trend for hospitals to plant drought-tolerant landscaping or native vegetation instead of turf grass to save water. The ASHE/AHE/HFM survey supports Huff's observation. Of the survey respondents, 35 percent say they have implemented drought-resistant landscaping in the past two years and another 13 percent plan to implement it in the next two years.
Green cleaning
Hospitals are lagging in adopting green cleaning initiatives compared with other key areas of sustainability, but evidence shows that may be improving. While only 30 percent of hospitals in the ASHE/AHE/HFM survey said they measure savings from the use of sustainable cleaning practices, there is strong growth in the use of environmentally safe products.

In the last two years, 81 percent of survey respondents said they use microfiber mops and cleaning cloths to reduce water and chemical use. And 78 percent say they use cleaning equipment that does not negatively impact indoor air quality.
Practice Greenhealth's 2010 Sustainability Benchmark Report provides more positive news on sustainable cleaning. The report summarizes data collected from the 2010 Environmental Excellence Awards applications and contrasts the Environmental Leadership Circle (ELC), the highest level of winners, with the Partner for Change (PFC), the main level of winners.
The report says 67 percent of the ELC winners, who were recognized for their green cleaning and other initiatives, have developed a formal green cleaning program. The report says 54 percent of the Partner for Change-level winners have established a formal sustainable cleaning program. "The fact that hospitals are formalizing their green cleaning programs is relatively new," says Hill of Practice Greenhealth. "In the last five to 10 years, green cleaning has become more of a priority and more products are available."
The report also says that 96 percent of the ELC winners and 83 percent of the PFC winners have collaborated with their respective infection control committees to identify areas where use of disinfectants can be minimized or eliminated. Hill calls this an important development.
"It's expensive and time consuming to over clean and it's dangerous to under clean," says Hill. "These numbers are significant because it shows improved communication within the hospital."
Jeff Ferenc is senior editor for Health Facilities Management.





