Technical requirements for 96-hour preparedness
Emergency preparedness underscores the importance of being resilient and able to adapt in the face of adversity.
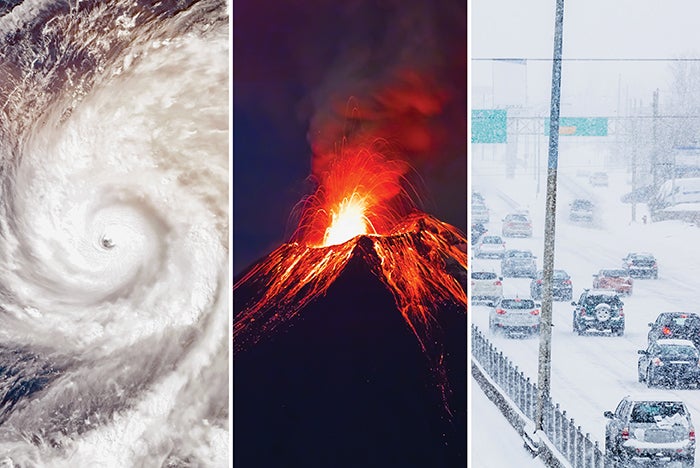
Images by Getty Images
Surveyors representing the Centers for Medicare & Medicaid Services (CMS) or an accrediting organization (AO) evaluate whether health care organizations meet the emergency preparedness requirements of the Conditions of Participation (CoPs).
These requirements assess the extent to which an organization is prepared for various emergencies as determined by their Hazard Vulnerability Analysis (HVA).
Unique scenario
Imagine a health care facility in a remote area between three volcanoes. That scenario applies to one facility noted for its excellence in emergency preparedness. Each health care facility’s HVA is unique, in the same way that each health care facility’s location and access to materials, supplies, fuel, water and food during an emergency are unique.
The hospital recognizes that the likelihood of a volcanic eruption is low, but the risk to the facility and its occupants is high given its location. Thus, it scores high-risk on its HVA.
“It will probably never happen in our lifetimes,” remarks an emergency management committee member at the hospital, “but if it does happen, we will most likely become ‘an island’ out here.”
A volcanic eruption is a scenario they have actively prepared for, detailing the emergency response procedures in their emergency operations plan (EOP) and conducting emergency response drills to educate and train staff on what to do if it were to happen.
One thing that stands out is how much food, water, fuel and emergency supplies have been stored by the hospital’s staff. But given their explanation of the risk to the facility during a volcanic eruption — or other emergency or disaster — and the remoteness of the location, it makes sense for them.
All organizations must decide what their response will be during emergencies or disasters and develop their EOPs accordingly. The decision regarding what and how many resources and supplies to store is made during emergency response planning by the organization itself.
Organizational decision
Health care facilities exist to provide medical care to patients under many conditions and sometimes elect to provide spaces that offer a community benefit during a disaster as well. The degree to which a facility needs to maintain continuity of operations depends largely on the decision of the organization and how it plans on maintaining services in an emergency.
A large medical center with multiple high-risk patients may need to sustain most of its operations, but a smaller rural or specialty rehab hospital with low-risk or swing-bed patients may decide that evacuating is its best response. Even if the plan is to evacuate to another facility, it takes time and planning, and facilities will need to at least remain partially functional until the transfer happens or supplies can be replenished.
For facilities that receive CMS funding, the requirements for emergency preparedness are included in the CoPs, Part 482.15. Additional guidance for compliance with the CoPs for all types of health care facilities, including hospitals, long-term care facilities and critical access hospitals (CAHs), among others, is provided in Appendix Z of the State Operations Manual.
Within Appendix Z, the emergency preparedness requirements describe the comprehensive standards that health care organizations must follow to maintain readiness for unforeseen events, ranging from natural disasters to pandemics: “Facilities must be able to provide for adequate subsistence for all patients and staff for the duration of an emergency or until all its patients have been evacuated and its operations cease. Facilities have flexibility in identifying their individual subsistence needs that would be required during an emergency. There are no set requirements or standards for the amount of provisions to be provided in facilities. Provisions include, but are not limited to, food, pharmaceuticals and medical supplies.”
In addition, being adequately prepared entails having reserves of other essential resources, such as fuel for emergency power sources and water to maintain appropriate care for patients. During an emergency, the level of care provided should be determined by the organization and documented in its continuity of operations plan (COOP) within its EOP. Resources and assets identified as essential need to be appropriate for the plan. Depending on the unique features of the facility, such as its location and access to community resources, the facility may elect to arrange for other methods of acquiring these resources and assets during a disaster event.
Regulatory requirements
So, where does the “96-hour rule” come from? The CoPs don’t require a hospital to have 96 hours of resources on-site. The AOs have standards that require hospitals to plan for the first 96 hours, but they don’t require the organization to remain operational or have resources on hand for the first 96 hours. For instance, DNV Healthcare USA Inc.’s National Integrated Accreditation for Healthcare Organizations requirements refer to the National Fire Protection Association’s NFPA 99, Health Care Facilities Code, for guidance on emergency planning. PE.6 (SR.2), states, “The organization shall meet the requirements set forth in NFPA 99 (2012), Chapter 12, Emergency Management, and the requirements of PE.6 (SR.3-5).”
The 2012 edition of NFPA 99 includes requirements that the organization maintain a current, documented inventory of the resources it has on-site that would be needed during an emergency. These could include medical, surgical and pharmaceutical resources, as well as water, fuel, staffing, food and linen.
Once the inventory is established, the organization needs to identify which and how many resources they lack to sustain operations for 96 hours. It must then plan mitigation efforts to address any shortfalls. Lastly, the organization must monitor the quantity of assets on a continuous basis.
While NFPA 99 mentions 96 hours, it doesn’t direct organizations to provide 96 hours’ worth of inventory, only to assess their shortfalls and determine if any mitigation is necessary. It also introduces the notion of “feasibility,” further stressing that if remaining open is not feasible for any facility, they have the option to evacuate.
The Joint Commission’s “Comprehensive Accreditation Manual for Hospitals” sets forth its own expectations, which also refer to 96 hours. Standard EM.12.02.09, EP 3, requires hospitals to develop a plan for managing their resources and identify what would be needed for 96 hours of operation based on their current usage. It clarifies that hospitals are not required to stay operational or stockpile all the assets needed to sustain operations for 96 hours. It also addresses conservation of resources through rationing, canceling elective procedures and redirecting for other needs.
Again, similar to NFPA 99 and the DNV expectations, The Joint Commission requires the organization to assess the first 96 hours and develop a plan but does not require it to have 96 hours’ worth of resources or to remain fully functional during the first 96 hours.
Regardless of the applicability of accreditation standards, facilities must engage in collaborative efforts with community partners, emergency management agencies and public health entities to allow for coordination and mutual support in times of crisis. This includes establishing agreements for resource sharing, memorandums of understanding with suppliers, evacuation protocols and communication channels to facilitate seamless response and recovery efforts.
For all hospitals, regardless of whether they participate in Medicare or Medicaid or are accredited by DNV, The Joint Commission or others, emergency preparedness underscores the importance of being resilient and able to adapt in the face of adversity. By adhering to stringent emergency preparedness expectations, organizations can mitigate the impact of disasters, safeguard the continuity of care and protect the welfare of patients and staff. This ensures compliance with regulatory requirements and develops a preparedness mindset, ensuring that patients, staff and visitors are adequately cared for.
Maintaining emergency power
Questions frequently arise, accompanied by occasional misunderstandings, regarding the necessity of storing generator fuel on-site. There are two parts to determining this for any organization. The first part is defined by code and includes determining how much fuel is required to sustain the “class” rating of the emergency power supply system (EPSS). The second part is an organizational decision. This includes deciding whether the facility elects to store more fuel than required by its class to support continuity of operations.
Generators that are part of an EPSS are categorized by class, which indicates “the minimum time, in hours, for which the EPSS is designed to operate at its rated load without being refueled or recharged,” according to the 2010 edition of NFPA 110, Standard for Emergency and Standby Power Systems. For hospitals and CAHs, NFPA 99 requires them to be designated as Class X, which specifies the minimum runtime as “other time, in hours, as required by application, code or user.” This is a code minimum, and organizations may elect to plan for a runtime beyond the class requirement based on the needs of the COOP. There may be other factors that will determine a different class for a facility.
Although most facilities utilize diesel fuel for their generators, some use natural gas, requiring analysis of the need for an on-site alternate fuel source. According to NFPA 110-2010, Section 5.1.1, generator installations in areas prone to potential interruptions in off-site fuel supplies, like natural gas-fueled generators in seismic areas, must maintain on-site storage of an alternative fuel source. This backup fuel needs to be adequate to sustain the full output of the emergency power supply (EPS) for the specified class. In a hospital’s case, Class X is the duration the organization determines.
Facilities are required to have enough fuel on-site to meet the class of the EPSS, but they are permitted to refuel to sustain a continuity of operations. Limitations and delays in refueling should be considered during development of the COOP. Arrangements should be made to ensure that the designated fuel supply will not be compromised by other community demands during the same emergency. In cases when a facility plans to evacuate during an emergency while maintaining non-site fuel sources, a contingent amount of fuel should be retained to sustain the EPS until evacuation is completed.
Questions to consider
Careful planning is required for all facilities regardless of size, remoteness, and types and acuity of patients. Empowering the emergency preparedness committee and other staff to be part of what are often leadership decisions will help to ensure that the organization knows what its responsibilities, capabilities, liabilities and assets are. It will also allow staff to ensure that the organization is adequately prepared.
When planning for the first 96 hours or more after an emergency or disaster event, several further questions must be considered:
- What service does the facility provide to the community, and how long does it need to remain open in an emergency? That duration should be the focal point of the rest of the decisions. Consider the continuity duration for the rest of the questions below.
- What are the results of the HVA, and which emergencies (natural or man-made) require further study of the available resources? Do any of those impact (exceed) the continuity duration? Does the class need to be increased?
- What are the emergency response procedures for those emergencies? Do those response procedures need resources? Does the response require a duration that exceeds the class?
- What resources will be needed to ensure a continuity of operations, including medical supplies, medical gases, pharmaceuticals, linens, food, potable and non-potable water, and fuel for emergency power, heating and cooling?
- Will obtaining any of those resources take longer than the duration the organization has set? Do they need to change the class, or are there other mitigating factors that need to be considered?
- What is the current inventory of those resources? How long will that inventory last given normal usage? How about if the organization is at surge capacity?
- What resources are feasible to replenish over the duration decided by the organization?
- Can the organization conserve resources if needed?
- What impacts do the location of the facility have on the organization’s ability to acquire resources from outside partners in case of an emergency?
- Can the organization depend on these outside partners to supply the resources they might need?
- Do the organization and outside partners need to stockpile more resources in case of an emergency event?
After these factors are considered, facilities professionals should consider the longest duration the organization can, or plans to, accommodate services in an emergency. They should plan all the resources and mitigation strategies for that duration. If it’s under 96 hours, the plan can terminate when the organization has closed the facility.
Once the inventory of needed emergency reserve supplies has been established, the organization must also consider the degree to which those supplies need to be maintained when not in an emergency.
Many of the supplies may routinely expire. By continuing to use the reserve supply during normal operations and replenishing them as needed, organizations can keep their supply refreshed and prepared for emergency or disaster events.
Empowering staff
For many facilities, the goal of emergency preparedness is to ensure a continuity of services without disruption. Additional consideration will need to be given to ensure readiness for the first 96 hours and beyond.
While the focus for CMS and AOs is on the first 96 hours, given the unique needs of the organization, they may need to plan beyond that, or they may decide to transfer patients and cease some operations. Each facility is unique in its needs, so it is important to plan accordingly.
Ultimately, empowering staff and thoughtful planning enable organizations to fulfill their responsibilities and commitments to the communities they serve, ensuring that they are always ready to face whatever challenges may arise.
Understanding ‘class’ ratings for hospital emergency power
In the context of the National Fire Protection Association’s NFPA 110, Standard for Emergency and Standby Power Systems, the term “class” refers to the “minimum time, in hours, for which the emergency power supply system (EPSS) is designed to operate at its rated load without being refueled or recharged.”
NFPA 110 specifies different classes to categorize EPSSs based on their duration of operation. Here is a brief overview of the classes applicable to health care facilities as defined by NFPA 110:
- If a facility is a high-rise building, it must have a Class 1 (60 minute) EPSS as a minimum, according to the 2012 edition of NFPA 101®, Life Safety Code®, Section 11.8.5.3.1.
- If a facility is new (since July 5, 2016) and has emergency lighting or illuminated exit signs that do not have battery backup for at least 1 ½ hours, then it must have a Class 1.5 (90 minute) EPSS, according to NFPA 101-2012, Sections 7.9.2.2 and 7.10.5.2.1.
- If a facility contains a smokeproof enclosure, any new mechanical ventilation equipment (since July 5, 2016) requires a Class 2 (120 minute) EPSS, according to NFPA 101-2012, Section 7.2.3.12.
- If a facility contains a fire alarm or emergency communication system, the components of that system and any fire supervising stations (if applicable) must have a Class 24 (24 hours) EPSS, according to the 2020 edition of NFPA 72®, National Fire Alarm and Signaling Code®, Sections 10.5.10.3.1.1 and 10.5.10.3.2.
- All health care facilities that contain Category 1 or Category 2 spaces (as defined by NFPA 99, Health Care Facilities Code, Chapter 4, Fundamentals) shall have a Class X EPSS. Class X is a custom class, where the duration is specified by the user based on its needs or requirements beyond the defined classes.
When choosing the appropriate class for the EPSS, the class designation does not have to match the continuity of operations plan.
The class of EPSS is crucial for determining the minimum duration that a power source will provide power during an outage. This is essential for planning, especially in critical applications such as hospitals and other facilities where continuous power is vital.
About this article
This is the second in a two-part article about 96-hour emergency preparedness. This piece delves into technical requirements of emergency preparedness and how health care organizations can comply. The first piece introduces the concept of a 96-hour plan and dispels longstanding myths about stockpiling supplies and other resources.





