Hospital technology and healing spaces

A carefully developed vision and strategy is required for planning, designing and constructing a smart hospital or renovating an existing facility with technology.
Image by Getty Images
In today’s rapidly evolving health care landscape, the integration of technology into the planning and design of care environments has become paramount. The convergence of health care and technology is transforming the way care is delivered and improving overall outcomes. However, the holistic impact on the care experience and user experience for both patients and staff remains unclear.
Over the last two years, The Center for Health Design and its Environmental Standards Council (ESC) have begun to explore this topic. They’re looking at how design teams are planning for current and future technology needs and evaluating their impact on the functional operation of the health care delivery system, the care environment and the overall patient and care team experience.
After much review and study of the rapidly increasing use of technology in health care facilities (particularly after the COVID-19 pandemic), the ESC believes that much more attention is required to assess technology’s impact on the operational and physical design of today’s health care facilities.
A crucial role
Technology has revolutionized various aspects of health care — from managing a building’s physical environment and providing diagnostics and treatment, to patient management via electronic health records (EHRs) and care team communication.
In the context of health care design, technology plays a crucial role in creating environments that are not only functional but also conducive to healing and well-being. This extends beyond clinical operations and into the overall building management system, providing monitoring and automated controls for individual systems that positively contribute to the sustainability and resilience of the facility.
More recently, the integration of advanced technologies such as telemedicine, wearable devices and smart hospital rooms have shown the potential to enhance patient care, streamline workflows and improve the overall efficiency of health care facilities.
A primary goal of incorporating technology into health care design should be to enhance the patient and care team experience. Often, the patient experience begins before the patient arrives at a physical location and involves interacting with a technology that facilitates the initial interaction, such as a website or app for scheduling and/or registration. Technology then continues to intersect with the patient experience at a high frequency across the care continuum and is only increasing with new advancements.
Health care organizations are increasingly focused on creating patient-centered environments that prioritize comfort, safety and convenience. Telemedicine, for example, allows patients to consult with health care providers remotely, reducing the need for physical visits and minimizing travel-related stress.
Wearable devices enable continuous monitoring of vital signs, providing real-time data to health care professionals and empowering patients to take an active role in managing their health. While telemedicine and wearables are not new, they are continuing to revolutionize care in new ways that create regular technology touchpoints for patients and the care team.
Smart hospital rooms equipped with advanced experiential technologies can automatically adjust lighting, temperature and other environmental factors based on patient preferences and even ambient listening controls, creating a more personalized and comfortable experience.
Additionally, advanced imaging technologies, artificial intelligence (AI), virtual monitoring and EHRs streamline diagnostic and treatment processes, reducing wait times, increasing throughput and improving the accuracy of medical interventions.
Multidisciplinary programming
Too often, technology is an afterthought in facility design, subject to inadequate planning. The successful integration of technology into health care design requires a collaborative approach involving a multidisciplinary team.
During the functional programming phase, architects, engineers, health care organizations, information technology (IT) specialists and other stakeholders work together to define the requirements, objectives and the project budget. This phase is critical for identifying the specific technological needs of the facility and ensuring that the design aligns with the goals of the health care organization while also enabling future considerations.
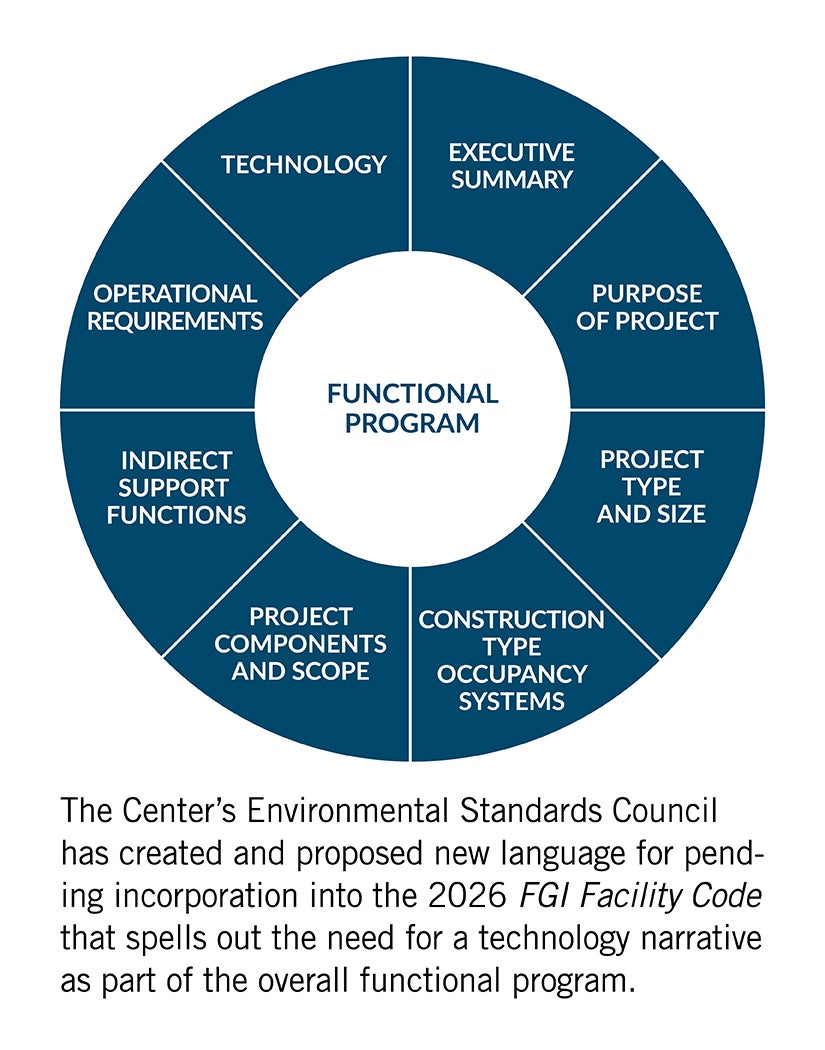
The Facility Guidelines Institute’s 2026 FGI Facility Code may further reinforce this with the pending incorporation of language — created and proposed by the ESC — spelling out the need for a technology narrative as part of the overall functional program.
A clear technology narrative that is carefully developed and maintained should ensure that systems are integrated and operationally compatible throughout a facility’s useful life. The pace of technology development makes it impossible to predict future innovations, underscoring the importance of maintaining an up-to-date technology narrative to inform the consideration, design and efficient implementation of initiatives yet to come.
Collaboration among team members fosters this holistic understanding of the project, allowing for the identification of potential challenges and the development of innovative solutions. For example, IT specialists can provide insights into the infrastructure and supporting applications needed to assist advanced technologies, while health care providers can offer perspectives on how these technologies can enhance patient care and improve clinical workflows.
By involving all relevant stakeholders from Day 1 of the planning process and continuing to engage them throughout the design and construction life cycle, health care facilities can create environments that are technologically advanced, patient-centered and care-team centered.
Because technology in today’s health care journey and experience plays a role from the time a patient, family or care team leaves home and returns home, technology should play a role in designing the arrival experience, entering a lobby, navigating the path to care, providing continuous real-time awareness, discharge and hospital at home.
All elements of the physical environment should take into consideration how technology can enhance or detract from the experience while improving efficiencies and quality of care. Realizing the role of technology from the start will ensure an integrated care delivery model that encompasses all facets of care, not just its delivery. The design of the building operations, security, facilities and lighting must be integrated to ensure the experiential goals are met.
Moreover, technology must align to ensure a welcoming environment for not only today’s patients and care team members but also for generations to come.
Proactive planning
Incorporating technology into health care design is an ongoing process that requires proactive planning. As technology continues to evolve, both new and existing health care facilities must be designed for flexibility and adaptability. This means anticipating future technological advancements and ensuring that the physical environment can accommodate new innovations without significant disruptions.

A multidisciplinary team is needed for proactive planning and successful integration of technology into health care design.
Image by Getty Images
One approach to proactive planning is adopting modular and scalable infrastructure. For instance, structured cabling systems that support multiple applications can be easily upgraded or reconfigured to accommodate new technologies.
Similarly, flexible spaces that can be repurposed for different functions allow health care facilities to adapt to changing needs and technological advancements. Health care organizations must strike the right balance of integrating applications and standardizing them when possible to build a scalable plan while being fiscally smart.
Another important aspect of proactive planning is the consideration of cybersecurity and data privacy. With the increasing reliance on digital technologies and EHRs, health care facilities must implement robust security measures to protect sensitive patient information, in addition to increased measures to protect building and security controls. This includes not only technical solutions such as encryption and access controls but also policies and procedures to ensure compliance with regulatory requirements.
Additionally, each individual technology’s impact on space must be considered — not only the size of the infrastructure to accommodate future changes but also the technology itself.
Master plan and vision
Ultimately, the technology narrative and functional program may evolve into a technology master plan that provides a flexible framework for the adoption of new and future technologies.
Health systems are inundated with the latest and greatest advancements or gadgets that may or may not be beneficial to their communities, organizations or patient populations. These must be filtered through the needs of each health care organization and aligned with their overall capital and operating budgetary constraints.
With the proliferation of technology increasing each day, it is essential that design professionals understand which technology components are proposed for new facilities and which existing technologies are already in use by the health care organization. All members of the multidisciplinary team will benefit from having this information available to them during planning, design and implementation.
This master plan would provide a lens through which to evaluate these exciting new technologies, and a business case could be developed considering how they may impact patient care, staff operations, revenue and reimbursement, or other target measurables.
Additionally, a successful master plan addresses the entire life cycle of technology, from concept through evaluation and design to deployment and operationalization. These impacts extend to supporting applications for these technologies to address downtime and troubleshooting. Organizations must accommodate this not only from a budgetary perspective but also through appropriate staffing and resourcing of experienced technicians.
It will be increasingly essential to have an accurate inventory of such systems over the life of the facility so that informed decisions can be made regarding new systems proposed and/or innovated. Furthermore, the initial cost of such a narrative will be commensurate with the scope and scale developed by the project team and likely included in initial programming and planning efforts.
An understanding of the overall scope and scale of technology will provide an increasingly valuable cost benefit to future projects at the facility.
Design guidance
The journey of planning, designing and constructing a smart hospital — or renovating an existing facility to leverage technology — is a huge undertaking. Having a carefully developed vision and plan and a dedicated team of stakeholders make it less daunting and more achievable — and design professionals may discover they already have some tools and resources at their disposal.
Some key approaches include the following:
- Remember the entire patient, family and care team journey embraces technology, not only in design but also in the experience.
- Focus on the technology experience from Day 1.
- Invest time in current state discovery of technology and how it’s impacting care delivery to maximize investments.
- Create a technology vision, journey or experience and embed that process early and throughout the design life cycle.
- Ensure the technology planner or IT team understands the experience and future alignment to key goals and outcomes.
- Identify who owns the technology integration, implementation, commissioning and activation.
- Realize the technology budget is not only “low-voltage items” and standard equations.
Impact on care
The integration of technology into health care design is driving the development of new care delivery models that prioritize efficiency, accessibility and patient-centered care.
For example, the rise of telemedicine and remote monitoring has enabled health care organizations to deliver care to patients in their homes, reducing the need for hospital visits and improving access to care for individuals in remote or underserved areas. Likewise, virtual nursing is reinventing the acute patient care staffing model, reducing the cost of care, bridging the staffing gap and improving the quality, safety and efficiency of bedside care. Furthermore, technology-driven innovations such as robotic surgery and AI-powered diagnostics are enhancing the precision and effectiveness of medical interventions.

Technology’s integration into health care design is driving the development of new care delivery models such as telemedicine and remote monitoring.
Image by Getty Images
These advancements are not only improving patient outcomes but also reducing the burden on health care organizations by automating routine tasks and enabling more efficient use of resources.
Incorporating technology into the planning and design of health care environments is essential for creating facilities that are responsive to the needs of patients and health care organizations. By involving a multidisciplinary team in the functional programming phase and proactively planning for current and future technologies, health care organizations can create environments that enhance patient experiences, improve clinical outcomes and support the delivery of high-quality care.
Technology is no longer just a component of the environment of care, but it also is driving the development and evolution of the environment of care. The incorporation of technology into the planning and design of health care environments is a non-negotiable for creating facilities that are responsive to the needs of patients and health care organizations. To best serve the users of these technologies, designers must enhance communication, ensure integration and guide innovation.
Related article // The Center for Health Design’s Environmental Standards Council
Since 1996, the Environmental Standards Council (ESC) has been a subcommunity of The Center for Health Design, seeking to ensure that The Center’s mission of maximizing health through informed design is acknowledged and understood by various oversight entities guiding and regulating health care design.
This multidisciplinary group of 18 current volunteer members — health care facilities executives, design professionals, regulatory agencies, product manufacturers and educators (some of whom have served since the ESC’s original inception) — seeks to accomplish its mission by presenting its work at conferences and providing regional educational sessions.
The council’s most recent accomplishment is the development of an online Functional Program Process Guide tool, utilizing the Facility Guidelines Institute’s (FGI’s) functional programming format to assist project teams with federally mandated functional programming requirements.
The tool details the five steps to create a functional program that will communicate an owner’s project requirements to the entire project team; meet applicable regulatory requirements for design and construction; and optimize a project’s design and leverage the physical environment to improve patient outcomes, staff effectiveness and sustainability.
The ESC also has worked with FGI as a coauthor in developing and updating the “Environment of Care” chapter in the 2006, 2010 and 2014 editions of its Guidelines documents. Additionally, this group has collaborated to support the work of The Joint Commission and other accrediting and regulatory agencies.
For nearly three decades, the ESC has sought to ensure that the evolving provision of care and care environments continue to benefit from The Center’s ever-increasing provision of guidance through applicable research and resources. This diverse group of health care experts is committed to ensuring that the human element of providing health care is a primary consideration during planning, programming and design of the settings in which that care occurs.
For more information on the ESC and the Functional Process Program Guide tool, access The Center's website.
About this article
This feature is one of a series of articles published by Health Facilities Management in partnership with The Center for Health Design. Authors of this article are members of The Center’s Environmental Standards Council (ESC). To learn more about the ESC and The Center’s other professional groups, visit their website.
Chase Miller, AIA, ACHA, EDAC, is a senior health care planner at Guidon in Indianapolis, and Corey Gaarde, FHIMISS, CPHIMS, is a principal and project executive for IMEG’s health care information technology advisory services team. They can be reached at cmiller@guidon.com and corey.m.gaarde@imegcorp.com.