Sizable difference
 |
|---|
Photo by Jeffrey T. O’Neill, AIA, ACHA Nurses must be provided with a number of work areas. |
A common challenge for health care designers is convincing administrators and clinicians that space requirements for a given function have increased over the years.
Most existing hospitals still use at least portions of their physical plants that were constructed before the 1970s. Since then, of course, layers of regulations have been added that influence how spaces are constructed.
Over time, codes and guidelines that affect hospital construction have been issued by the federal government, Facility Guidelines Institute (FGI), International Building Code, National Fire Protection Association, and federal and state departments of health, among others.
Also, changes in technical and medical protocols have become a constant aspect of the dynamics of health care. In addition, focus on increased safety in inpatient settings has fueled further changes in space needs.
Understanding these changes is key to navigating the effects on the owner and user groups when designing new health care spaces.
Compelling challenges
While the impact of these changes can be seen throughout virtually all clinical spaces within a health care facility, some key examples trace compelling challenges in modifying, replacing and upgrading existing facilities.
Inpatient units. Gone are the days of the 16-bed open wards that gave patient care staff unobstructed observation of an inpatient from a single dominant nursing station. These have been replaced by a variety of double-loaded corridor configurations, "T" configurations and racetrack plans. The shift to a single-patient room model for most inpatient care units comes with a significant ripple effect that aggregates the total space needed. Space within the room itself frequently exceeds the minimum prescribed square footage in guidelines, driven by minimum clearances as well as a response to an increasing application of family-centered care models, including Planetree principles.
Within the room, requirements now include clinical "touchdown" space, including a sink, storage and charting in the room at a stationary location; these functions are preferably maintained free of space dedicated for family. Outside the room, the 8-foot-wide corridor now needs to remain clear, so alcoves are needed to stage medical equipment. Along with the decentralized nurses' stations driven by a single-room model, more space is required for soiled and clean utility areas, and information technology closets.
The impact of these changes can create a demand of 30 to 50 percent more space per bed as comprehensive renovations are contemplated; in some circumstances where existing environments are quite dated, the ratio of space demand per bed may be more than double the existing space provision.
About this articleThis feature is one of a series of quarterly articles published by Health Facilities Management magazine in partnership with the American College of Healthcare Architects. |
Emergency departments. Ambulatory care and surgeries have replaced the emergency department (ED) as a feeder to the hospital. With those changes in mind, the ED has become an area of specialized care, including increasingly specific requirements for trauma. In addition, the need to respond flexibly to a range of patient care demands has caused many institutions to use a single-room model that has become larger because of increased clearance criteria.
These include concerned family members who accompany a patient in an emergency situation and the amount of equipment that is necessary to deliver a wide range of emergency care, including ventilators, imaging and monitoring equipment. Again, quality of care and efficiency of "flexing" acuity of care within the unit is possible at the cost of more space. Similar to inpatient bed units, the drive to a private-room model has an ancillary impact on decentralized nursing models and related support elements.
An offshoot of the ED has been the development of an observation unit for a 23-hour stay. This creates an entirely new type of space and finding a suitable location is a challenge for the institution. With the emergence of this subset of clinical care, characteristically driven by patients arriving at the ED, there is further pressure and demand for additional space.
Delivery of nursing care frequently results in charting at nurse servers, satellite stations, in the patient's room or at a hub or central station. While redundant clinical documentation sites address the flexible needs of clinicians, they result in more dedicated, frequently scattered space for this function. In most cases, all areas need to be available. This eases the ebb and flow of patient room availability in response to daily and weekly patient census spikes.
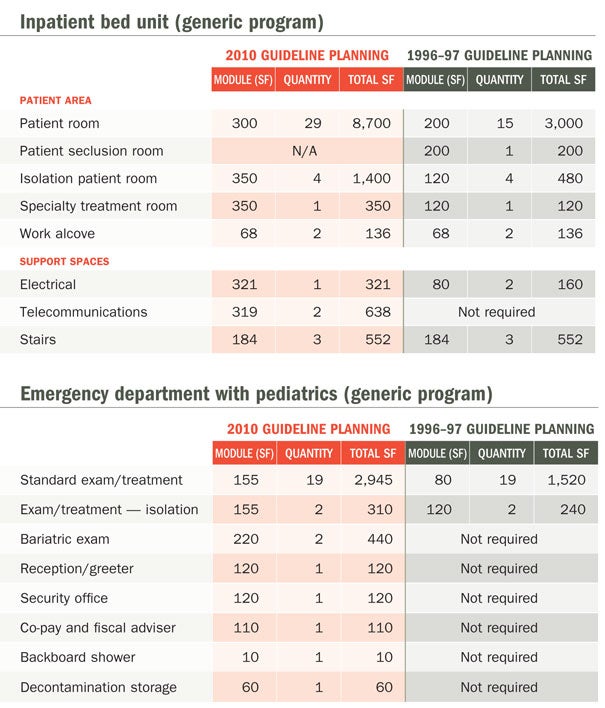
As noted in the programming charts on Page 32, there are numerous required elements due to regulatory mandates and not strictly due to direct patient care.
Financial and consultative privacy must be maintained because of HIPAA standards, and require separate consult rooms. Similarly, decontamination areas were called for in the FGI's 2001 Guidelines for Design and Construction of Health Care Facilities, which created the need for independent storage and cleaning areas.
Diagnostic imaging. Advances in imaging technology and the increasing number of modalities have caused radiology departments to become very complicated areas. Aside from operational relationships such as proximity to the imaging department and in-suite or in-room surgical imaging, the technology itself has resulted in increased space demands for the equipment and the need for careful subdepartmental boundaries driven by patient safety protocols.
The American College of Radiology issued guidelines of their own for safe practices in relation to nuclear medicine and magnetic resonance imaging (MRI) patient care. For the MRI in particular, the definition of zones of safety was developed to make sure anyone with metal implants or sensitivities does not stumble accidentally into the magnetic field. Naturally, the distance buffers take more space and result in a thoughtful arrangement of the overall support spaces to the scan rooms.
Advances in modalities also have an influence on the amount of space imaging requires. Interventional radiology now requires surgical protocols including one-way flow staff access through dedicated lockers, distinct zones for sterilization and modality-dedicated holding for both inpatients and outpatients. These spaces previously were only required in the operating room (OR) environment.
Specialty market sectors, especially for women's imaging, need to be separated from normal imaging flow, eliminating the opportunity to share functions such as regular and gowned waiting areas, check-in and check-out spaces. Specialized technology also requires specialized staff and specifically tuned support space to accommodate their needs. Although the advent of computer technology seems to eliminate the need for records and film storage, the need for server space actually increases as information technology demands continue to grow.
Thus, the radiology department of 15 or 20 years ago is now replaced by a series of subdepartments that demand autonomy. Some imaging services, focusing on a specific patient subset may be completely isolated from their former location as part of a comprehensive diagnostic imaging department. Additionally, the adoption of a two-front door model that accommodates both inpatients and outpatients has an ancillary impact on circulation, control and arrival points and the creation of multiple inpatient holding and outpatient waiting zones.
 |
|---|
Table provided by the authors |
Additional impacts
Beyond these traditional benchmark areas, other portions of the clinical setting are bearing the challenge of parallel space increases because of technical criteria and design standards.
Surgical suites. Notable in OR suite planning are changes in demand for space within the surgical suite itself as well as in supporting patient care spaces, including:
• OR suites. The expansion of OR suite size has been the subject of considerable focus as selected procedures demand larger teams, equipment and diagnostic technology. In this instance, construction guidelines have been exceeded by pressures within the clinical community for more space, flexibility and a capacity for diagnostic imaging modalities and robotics. The old standard of a general OR suite at 400 net square feet (nsf) and a specialized OR suite at 600 nsf has been replaced in many settings by suites sized from 650 to 750 nsf, with some as large as 900 to 1,100 nsf.
• Ambulatory surgery holding or second-stage recovery zones. These areas have shifted from a "three drape and a headwall" paradigm to either a "three wall and a drape" or a private-room model. The latter two require significantly more space due to the requirements for side and end clearances and demand for hand-washing capabilities.
Maternity units. Changes in birthing units also have led to increased space requirements for maternity care, including:
• Postpartum inpatient bedrooms. Many institutions have shifted from a central nursery planned for a 1:1 ratio to a model of "laying in," which results in a reduction of space in a central nursery while increasing space within the postpartum bedroom to accommodate the infant as well as space for the infant's clinical care. While some of this may result in a straight swap of space, there usually remains a need for a central nursery with all of its related support elements.
• Neonatal intensive care units (NICUs). Construction guidelines have focused on radical shifts from the old open-ward plan for NICUs to either a large, semiprivate bay or a single-room model, in some cases magnifying the demand for specialized NICU care by a factor of three or four times the original ward. Evidence-based design confirms the value of a single-room model, but cost and space factors can lead to consideration of a semiprivate bay concept. However, in both cases, the demand for space has increased significantly in the last 10 years.
Endoscopy areas. A number of key areas in the endoscopy suite also have grown due to standards and technologies, including:
• Procedure rooms. There has been a resurgence of hospital-based endoscopy diagnostic volumes, driven by the need for this diagnostic tool among mid- to high-risk patients who are ill-suited to private-practice outpatient facilities. Thus, high-tech endoscopy suites are re-emerging within inpatient settings as part of the hospital's diagnostic and treatment space. The guidelines' requirements of a minimum of 200 nsf is exceeded by the technical demands of a room that must host a diagnostic team and anesthesiology with related support equipment, driving the room to a range of 320 to 360 nsf.
• Support areas. While holding area and post-procedure recovery needs can be modest, the move to higher-risk inpatient cases may result in the functional program driving additional space to allow for preparation via sedation and, subsequently, for more time in recovery.
• Bronchoscopy areas. Often, these spaces are collocated because of clinical efficiencies, and older clinical settings accommodated the pressure requirements of a bronchoscopy room by having the mechanical system shift from positive to negative. That protocol no longer is allowed, requiring a dedicated negative-pressure bronchoscopy room. This frequently causes a low utilization rate driven by a strong disparity between endoscopy and bronchoscopy volumes. Thus, the room remains substantial and, because of its mechanical-electrical-plumbing needs, underutilized.
These clinical components are not a comprehensive list but a starting point to explore the challenges created by the changing space standards and clinical paradigms facing consulting professionals or internal facilities planning and construction teams.
Impact on design
Although design regulations seem to be a set of rules that gets in the way of planning, they actually are concentrated wisdom to facilitate ready solutions before even meeting with a user group. Using them in this way brings credibility to the process, especially when dealing with senior administrators.
Space programming can be an essential opportunity to define compliance issues. Often neglected because of time or funding constraints, the proper use of an interactive planning process can promote the overall schedule, prevent backing up and help to frame a pragmatic solution prior to the development of test fits or schematics.
Clinical and administrative stakeholders can develop thoughtful solutions by reviewing basic compliance issues together. In addition, this re-frames meetings as work sessions to set the compliance issues and establish more specific operational issues to be left to the remainder of the design process.
Illustration of current clinical solutions that respond to current criteria and regulations can be a powerful tool in educating both administrators and clinicians on the nature of dynamic change that may have occurred since a unit or clinical service had been renovated or built.
These precedents also can help the team get past the spatial sticker shock that is a frequent result of early project scope definition.
Jeffrey T. O'Neill, AIA, ACHA, is director of engineering services at Penn Medicine/Pennsylvania Hospital in Philadelphia and Eric Lautzenheiser, AIA, ACHA, is director of health facilities planning at Francis Cauffman in Philadelphia. They can be reached at jeff.oneill@uphs.upenn.edu and elautzenheiser@franciscauffman.com, respectively.
Managing the costs of expanding health care facilities
Architects and planners can deploy several strategies to manage, contain and balance costs against operational benefits. They are:
• Consider the opportunity for gaining clinical efficiencies that can be tradeoffs for expanded space. This is particularly applicable in the implementation of a stand-alone room model that is replacing a function that used to be accommodated in semi-private settings. For example, can a single-room holding/Stage 2 recovery suite for ambulatory surgery serve as a site for parallel procedures? In one case, an institution has incorporated pediatric sedation magnetic resonance imaging (MRI) patients, thus eliminating the need for a microdepartment within the adjacent MRI suite while improving the quality of care for the patient. Subsequently, they have added several other two- to six-hour clinical protocols to the "Short Stay Unit," as it is now called. Another institution developed a private-room model that serves emergency department (ED) peak volumes in the afternoon and evening while serving the ambulatory surgery suite in the morning, thus maximizing the value of the capital expense by increasing its efficiency of use.
• Consider the complexities of a "blended" renovation, thus allowing the retention of selected elements of a grandfathered suite. This needs to be considered carefully by planners and clinicians alike but the judicious adaptive reuse of older clinical infrastructure for lower-acuity use may result in cost savings.
• Carefully explore the challenges and opportunities of decentralized clinical care delivery. This can be applied to inpatient bed units, EDs and other expanded clinical units by working with clinicians on "rightsizing" central nursing stations. The clinical impulse for comprehensive and sometimes redundant clinical space can drive support space needs up, while a careful exploration of clinical process flow may result in a right-size effort that maintains an appropriate balance of space.

