Never again
 The Institute of Medicine in 2006 estimated that 1.5 million patients are affected by medical errors, costing an average of about 2.4 million extra hospital days and $9.3 billion in excess payments.
The Institute of Medicine in 2006 estimated that 1.5 million patients are affected by medical errors, costing an average of about 2.4 million extra hospital days and $9.3 billion in excess payments.
These numbers prompted the Centers for Medicare & Medicaid Services (CMS) to investigate ways to help eliminate medical errors that should never happen, also called "never events." Moreover, this has led to pay-for-performance efforts, so that hospitals would not get reimbursed for instances in which a qualifying error has been identified.
National Quality Forum (NQF) in collaboration with Health & Human Services and CMS has been tasked with creating and implementing health care measures to report and improve adverse reportable events in health care. An NQF report published in 2002, revised in 2006 and currently being evaluated and maintained with possible updates is due out this year.
The report includes events within the following major categories: surgical, product or device, patient protection, care management, environmental and criminal. Within each category there are numerous adverse events.
The role of design
The hospital building industry and medical errors do not seem to have a common denominator until you start to evaluate the categories of adverse reportable events listed by NQF in which facilities design may serve an important role. These include patient protection, care management and environmental events.
Driven by data and statistics, the health care industry makes these three distinct categories the perfect zones of influence within the construction industry. Such process improvements as Lean and Six Sigma, evidence-based design and the U.S. Green Building Council's (USGBC's) Leadership in Energy and Environmental Design (LEED) for Healthcare (www.usgbc.org/DisplayPage.aspx?CMSPageID=1765) are tools that can be utilized during design in an effort to minimize the risk of medical errors.
Examining the three events
As one considers the following NQF events, one must evaluate the importance of participation and collaboration early in the design process and their influence in reducing the risk of medical errors.
Patient-protection events. As listed by NQF, patient-protection events include such situations as infants discharged to the wrong person, patient deaths or serious disabilities associated with patient elopement, or patient suicides or attempted suicides while being treated in a health care facility.
Suicide is the 11th leading cause of death in the United States, according to The Joint Commission Journal on Quality and Patient Safety. Studies have shown that delirium and confusion leading to depression in older adults may lead to suicidal thoughts while they are hospitalized and this can be partly attributed to cognitive impairment due to sleep deprivation. Addressing the environment is one method that potentially can help alleviate sleep deprivation. Studies have shown that interventions such as noise reduction, visibility of clocks and calendars, and provision of daylighting in patient rooms help mitigate confusion.
The facility can address noise reduction effectively through provisions of LEED for Healthcare Environmental Quality concepts specific to acoustic environments (Credit 2) that require health care facilities to provide a healing environment free of disruptive levels of sound. To this goal, facilities are to be designed according to the 2010 Guidelines for Design and Construction of Health Care Facilities by the Facility Guidelines Institute (www.fgiguidelines.org). A related document on the FGI website, "Sound & Vibration: Design Guidelines for Health Care Facilities," includes new guidelines for neonatal intensive care units in reference to exterior noise, acoustical finishes and room noise levels, sound isolation, paging and call systems and building vibration.
Daylighting in the patient environment is influential in reinforcing natural circadian rhythm to support alertness and sleep and wake patterns in patient sleeping or holding areas. Allowing variations of day and night lighting characteristics can influence delirium and confusion that could lead to the avoidance of depression and suicide. LEED for Healthcare Environmental Quality Credits 8.1 and 8.2, in reference to daylight and views, focus on daylighting of inpatient and non-inpatient areas with the purpose of addressing circadian rhythms. Furthermore, evidence-based design research has shown that provisions of windows in patient rooms have been credited to rapid recovery and reduced length of stay.
Other facility interventions for suicide prevention include eliminating risks such as grab bars, cords, sharp edges, artwork, furniture and sprinkler systems that can be used as anchor points by suicide-prone individuals. Careful selection of products like breakaway hardware, vandal-resistant mirrors and such design interventions as good visibility or windows into the patient rooms from decentralized nursing stations, which tend to be closer to the patient and with a direct view of the patient, also may be effective.
Other recommendations made by the Joint Commission include eliminating doors not required by code, removing doors from wardrobe units and replacing the rods with shelves, and removing linen and privacy curtains that can be used as nooses. A list of other environment-of-care recommendations can be requested from the Joint Commission via its website at www.jointcommission.org.
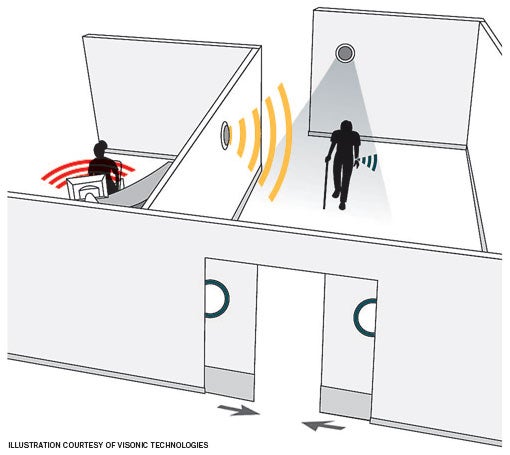 |
| This door-kit installation adds to patient safety by automatically closing the exit when sensors detect a wandering patient. |
Patient elopement and infant discharge have been addressed by health facilities through the utilization of tracking-system technologies that usually consist of a tag attachment to the patient or infant, featuring registration information input at the earliest possible time of contact with the patient. This tag generates an alarm if a mismatch or elopement occurs.
To minimize errors in this area, health care facilities rely heavily on information technology (IT). Consequently, facilities must be ready to accommodate infrastructure requirements to support these new technologies with dedicated space requirements for monitoring stations within the floor, coordination with door-alarm connections and closed-circuit television camera interfaces and all required maintenance interfaces that may be needed to support these new technologies.
It is highly recommended that facility professionals make sure that systems personnel and engineers know how new technologies interface with standard life-safety systems to minimize any risks. New monitoring technology needs to interface successfully with magnetic door locks, alarmed fire-exit doors, keypads and proximity card-entry systems that must be aligned with local and national egress codes and regulations for fail-safe, door-locking mechanisms during an emergency.
It also is highly recommended that IT representatives are involved early in discussions about user needs and product requirements for interfacing with a building's IT system. New technologies coming into the health care industry, such as electronic medical records and picture archiving and communication systems, require a robust network, more cable and more space above ceilings.
Often, IT representatives are brought into the discussions too late, which may cause IT rooms to be designed too small, not planned at all or stacked improperly within the facility. This also may result in lack of space above the ceilings for cable trays or any other IT needs. Other issues involve products and their infrastructure needs discussed late in the design process or during construction, causing an incredible number of interruptions.
Consequently, planning situations such as these are being addressed by LEED for Healthcare, with prerequisite points being earned for Innovation in Design (ID) Prerequisite 1: Integrated Project Planning and Design, ID Credit 3, where cross-discipline and design decisions are made during design programming. This would be in alignment with the most current productivity tool in construction project management, which is Integrated Project Delivery.
Care management events. As listed by NQF, care management events include patient death or disability associated with medication error, hemolytic reaction through administration of incompatible blood products, labor and delivery during a low-risk pregnancy, improper treatment of hyperbilirubinemia in neonates, hypoglycemia, pressure ulcers and spinal manipulative therapy.
Of course, all of the listed care management events cannot be attributed to health care facilities. However, some of the facility influence is driven by the Joint Commission through the caregiver process evaluation, which may influence how well facility design supports the caregiver process.
Proper evaluation and improvement of work process through quality improvement methodologies, such as Lean and Six Sigma, effectively can help mitigate a variety of events listed under this category. In this scenario, early collaboration among risk management, quality improvement and facilities design is beneficial.
The facility design team must collaborate as a unit with users and quality-improvement representatives by understanding the work process, providing all the proper physical requirements, removing physical barriers for that process to succeed and clearly understanding the ramifications of noncompliance, instead of having the process work around the physical plant.
Daylight, views and circadian rhythms also come into play in this category. LEED for Healthcare Environmental Quality Credit 8.1 references caregiver environments by providing an efficient lighting environment to support performance and alertness in both day-shift and night-shift lighting cycles to help prevent medication errors.
Equipment planning, as part of the project team, is tasked to listen to user needs, evaluate existing equipment, make recommendations on new equipment and follow up on a project budget. For instance, care management events like pressure ulcers may be alleviated by provisions of appropriate products such as patient beds to help relieve pressure.
Likewise, by staying abreast of new technology, product recalls, new product development and product research, the design team can help make recommendations that help the hospital avoid care management events. For example, evaluation of evidence-based design studies and recommendations on design interventions to help mitigate health care-associated infections, such as use of anti-microbial fabrics and properly located sinks, become critical in reducing the potential ramifications of infected open wounds.
Environmental events. Environmental events as listed by NQF include patient death or disability associated with electric shock, wrong or contaminated medical gas, incurred burns and patient falls while being cared for in a health care facility. This category is where facilities may have the most influence.
LEED for Healthcare Environmental Quality Credit 5 for indoor chemical and pollutant source control is an influential tool to aid in improvements to the patient environment to avoid potentially hazardous exposure to chemicals by patients, staff and community. This category addresses environmental quality through the development of a chemical-management policy that includes labeling products according to the Occupational Safety and Health Administration's hazardous communication standard.
This is used in such priority areas as dialysis, environmental services, facilities management and engineering, pharmacy, radiology, sterile processing, surgical services, laundry, laboratory, pathology, histology and nutrition services in favor of least-toxic alternatives to help minimize potential hazards.
Other influential LEED credits that can help minimize potential environmental events include the commissioning design-review process of the construction documents (Energy and Atmosphere Credit 3: Enhanced Commissioning) in alignment with the owner's project requirements for the different building systems. This would include electrical and medical gas systems during design, construction and at regular intervals thereafter.
Additionally, the Center for Health Design (www.healthdesign.org) has collaborated on research focusing on evidence-based interventions in response to patient falls with solutions such as slip-resistant flooring material, Americans with Disabilities Act-compliant grab bars, bars located within close proximity to bathrooms, alarms on patients who leave their beds, clear visibility from nursing units into patient rooms and the comparative benefits of centralized nursing units and decentralized ones, where caregivers are located closer or adjacent to patient rooms with a direct window view.
Three tools
The health care design and construction process and medical errors may not seem to have much in common until you consider the categories listed by NQF and evaluate whether facility design may serve an important role.
Process improvements, evidence-based design and LEED focus on operations of health care facilities. They are three tools that can be utilized successfully in various ways during the design and construction process to minimize potential medical errors.
Eileen D. Trimbach, AIA, LEED AP, BD+C, EDAC, is project manager at Moody Nolan Inc., Covington, Ky. She can be contacted at etrimbach@moodynolan.com.
| Sidebar - For more information |
| The following reference materials on "never events" and related health care patient safety and sustainable design issues were used by the author during the preparation of this article: • The Center for Health Design research • Facility Guidelines Institute 2010 Guidelines for Design and Construction of Health Care Facilities • Green Guide for Health Care Version 2.2 • "Joint Commission Alert: Suicides a Risk in the ER, Hospital," Nov. 17, 2010 • "Serious Reportable Events in Healthcare 2006 Update — A Consensus Report" •U.S. Green Building Council Leadership in Energy and Environmental Design for Healthcare |




