Decarbonizing for community health

A 750-kilowatt solar array on top of a University of Florida Health (UF Health) office park is one of the system’s many sustainability initiatives.
Image courtesy of Solar Impact
The first line in the American Hospital Association’s mission, “To advance the health of all individuals and communities,” emphasizes that the purpose of health care institutions extends beyond the hospital walls. Health care is fundamentally shifting to preventive care that maintains wellness as opposed to strictly treating disease. And, yet, the health care delivery system creates emissions that have adverse effects on the communities we serve.
The Centers for Disease Control and Prevention’s Climate and Health Program highlights that climate change interacts with other natural and human-made health stressors to influence human health and disease: “The health effects ... include increased respiratory and cardiovascular disease, injuries and premature deaths related to extreme weather events, changes in the prevalence and geographical distribution of food- and waterborne illnesses and other infectious diseases, and threats to mental health.”
But how big is health care’s contribution to climate-related stress? To put it in perspective, if the global health care sector were a country, it would be the world’s fifth-largest emitter of greenhouse gases (GHGs), according to a 2019 report produced by Health Care Without Harm. The global health care field is responsible for two gigatons of carbon dioxide (CO2) each year — the equivalent of 514 coal-fired power plants. The U.S. is the largest contributor to worldwide health care emissions in gross emissions and stands at 3.5 times the world’s average per capita health care emissions.
Based on a 2018 analysis by the American Council for an Energy-Efficient Economy, reducing conventional electric consumption by 50% in health care through efficiency or deploying renewables would have the impact of saving 180 lives and $1.6 billion in lower health treatment costs.
Committed to change
As scientists continue to document the health impacts of climate change, it is becoming clear that leadership in sustainable business practices is fundamental to the mission of health systems.
It is appropriate, then, that last year over 100 health care organizations signed onto the Department of Health & Human Services’ (HHS’) Health Sector Climate Pledge committing to lowering GHG emissions and building more climate-resilient infrastructure. The voluntary pledge includes that organizations will reduce emissions by 50% by 2030 (from a baseline no earlier than 2008) and achieve net zero by 2050.
Specifically, signers pledge to:
- Reduce organizational emissions by 50% by 2030.
- Achieve net zero by 2050.
- Publicly account for progress on this goal every year.
- Designate an executive-level climate leader by 2023.
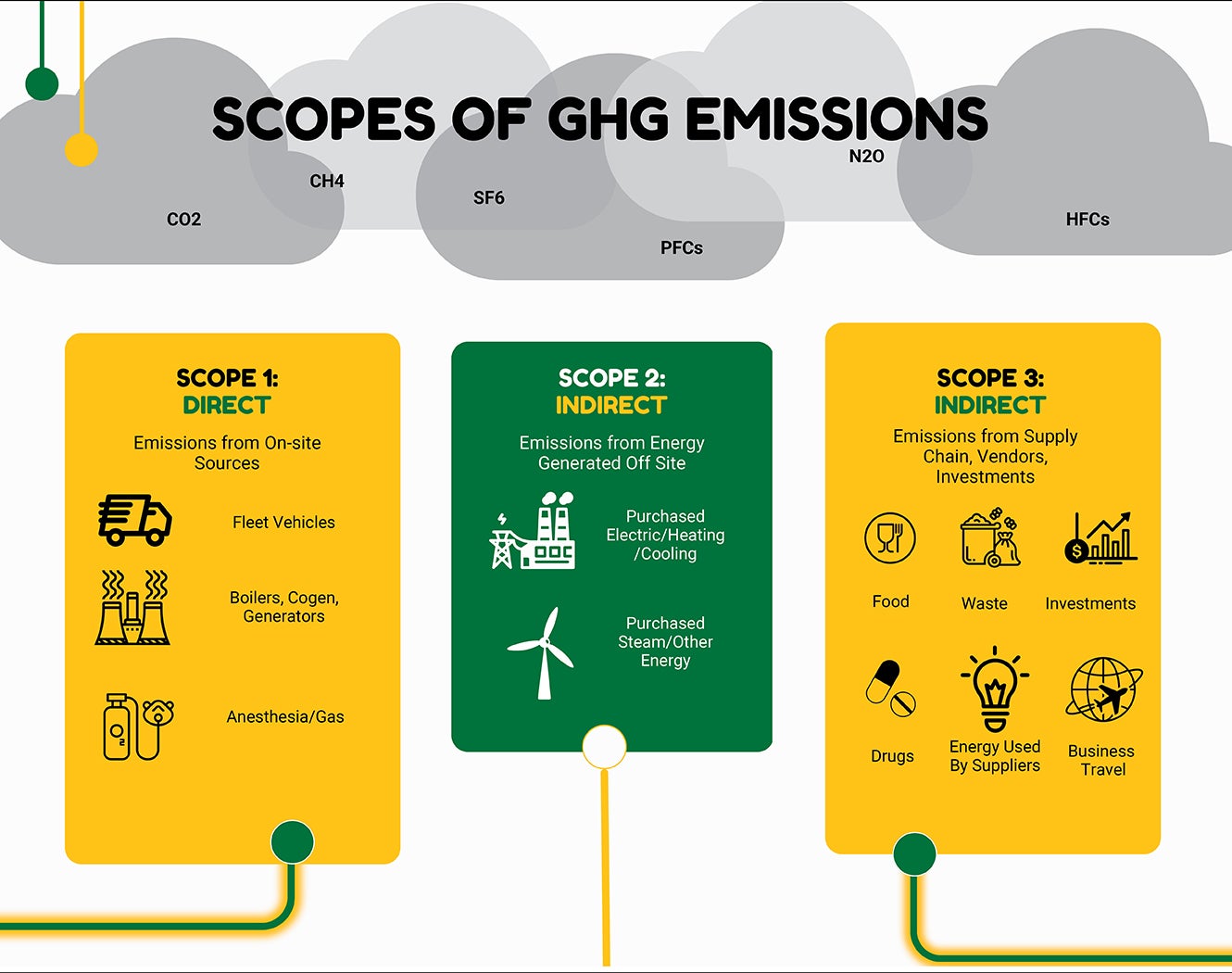
- Conduct an inventory of scope 3 (i.e., supply chain) emissions by the end of 2024.
- Develop and release a climate resilience plan for continuous operations by the end of 2023.
As health care systems look to make a significant impact on their GHG emissions, facility management teams are being asked to take a leading role by making the most immediate and visible actions toward sustainability.
For a health care organization’s GHG inventory, the internationally recognized GHG Protocol defines three scope areas, with scope 1 and scope 2 including emissions directly generated on-site from burning fossil fuels or escape of other GHGs like refrigerants, and indirectly from purchased utilities like district steam or purchased electricity (see graphic on page 50).
Health care facilities are among the most energy-intensive building types. The Energy Information Administration’s 2018 Commercial Buildings Energy Consumption Survey data show that health care facilities account for 9% of total energy consumption despite representing only 4% of total floor space.
Building energy use results in scope 1 and scope 2 emissions that facilities managers have direct control over. Additional sources of facilities management impact are water and waste, refrigerant management, vehicle fuel use, construction, and facility management tool and material purchases.
GHG emissions due to building energy use are among the easiest to quantify and track. By utilizing the EPA’s ENERGY STAR® Portfolio Manager® and ASHE’s Energy to Care® Dashboard, GHG emissions due to building energy use can be automatically calculated and tracked with progress toward commitments and return on investments demonstrated for both internal tracking and public reporting.
It is expected, then, that health care organizations will make the reduction of energy intensity of facilities a major emphasis in the commitment to eliminate GHG emissions in the sector. Demonstrations of success at the facility level can be much more visibly celebrated and form the foundation of broader initiatives.
Elevating facilities managers
As health care organizations rise to the challenge of leading in sustainable business practices, how do those involved with health care real estate and facility operations elevate their department’s role? One key ingredient is the executive team.
It’s become increasingly common for hospital executives to ask health facility leaders “What are we doing for sustainability?” and “What is our ENERGY STAR score?” The reasons are several: CEOs are concerned with market share and keeping up with best practices of corporate responsibility; CFOs are now seeing the cost of money is higher for those without a climate action plan due to environmental, social and governance reporting requirements tied to domestic and European investor pools; and COOs are concerned with cost reduction and operational excellence.
Whether sustainability is being driven top down or bottom up, executive team involvement enables greater results over the long run. By setting a vision, prioritizing objectives, allocating resources or monitoring progress, the executive team can do much to sustain the long-term commitment needed to achieve major carbon reductions.
To set a strong vision, the executive team should be part of reduction target setting, such as the HHS 50% reduction pledge by 2030.
To prioritize objectives and allocate resources, leadership should participate in creating a climate action plan. This defines what to do and in what order to work toward the reduction target.
Health care executives are used to working to improve numbers, and sustainability has plenty of metrics to give. Thousand British thermal units per square foot and ton of CO2 per patient-day are excellent lagging indicators to track performance.
Leading indicators that predict future performance include maximizing design chiller plant efficiency, targeting lower airflow per square foot and designing to achieve ENERGY STAR.
Across larger health systems, friendly competition can be a positive motivator for making big impacts. Sustainability initiatives need to be motivated and incentivized from the top, but the true work to make a difference comes from all levels of the organization.
To make the most of carbon accounting to drive change, health care systems should consider implementing their own carbon cost and use it to assess sustainability initiatives and decision-making for facility design and supply chain options. As an initial reference, the federal government now uses an interim value of the “social cost of GHGs” of $51 per metric ton of CO2 equivalent, which, to put in the context of energy, equates to an additional 2 cents per kilowatt-hour of average grid-supplied electricity.
Scaling up optimization
Facility operations offer immediate opportunities for significant carbon reductions that are both quantifiable and provide a good return on investment. For example, retrocommissioning existing building systems offer paybacks of two years or less and benefit reliability, comfort and compliance.
ASHE’s Energy to Care Program, along with programs like LEED and ENERGY STAR, has been supporting this journey with tools, certifications and awards. The program has grown to 234 hospitals, having received 10% to 15% reduction awards and over $500 million in savings. The Energy Information Administration’s most recent survey showed that while health care is the second most energy-intensive commercial building type, its normalized energy went down by 16% over the prior survey in 2012. How much opportunity is still on the table to truly have an impact? Even with the sector’s progress, only 4% of the nation’s hospitals have achieved an Energy to Care award, and only 6% (381) of all hospitals have been ENERGY STAR certified. Now is the time to scale up. The sustained commitment over the past 15 years of Energy to Care has demonstrated that awards yield further investment.
Today, capital upgrades that used to fall outside targeted hurdle rates are becoming more attractive when accounting for the cost of carbon offsets or solar generation that would otherwise be needed to achieve 50% and 100% reductions. Technologies like heat recovery chillers, energy storage, cogeneration and desiccant wheels are becoming a much stronger business case as a result.
The call for broad decarbonization also requires the measurement of operational optimization in areas such as water, waste, fleet, food and supply chain. Due to their success in energy savings, today’s facilities management professional is being asked to assist in resource optimization programs across several other functional departments, including environmental services, dietary, surgery and procurement.
Capital renewal and major construction projects within health care offer the next tier of opportunities in facilities departments. These projects provide the ability to change the game by investing in more efficient systems, and it is here that the goal of decarbonization can truly be realized. For example, utilizing heat recovery chillers and designing new facilities around hot water instead of steam for thermal heating can dramatically reduce a hospital’s need to utilize natural gas on-site.
Energy and carbon targets need to be incorporated into the owner’s project requirements from project initiation, giving architects and the rest of the design team clear direction in what constitutes project success. Energy targets should be explicit and based on actual first and second year of operation energy use, not just modeled performance. It is best to set objective criteria like an ENERGY STAR greater than 80 or a specific GHG emissions intensity target. Energy efficiency best practices such as those in the Energy to Care toolkit and the ASHRAE health care high-performance design guides should also be incorporated into project narrative documents.
Offset or generate?
Tackling conservation and efficiency opportunities will provide near-term reductions in GHG and are typically the quickest financial payback, and renovating or constructing high-performance buildings will reduce long-term energy intensity and provide life cycle cost benefits, but health facilities are always going to require energy for their operations. To close the gap toward the goal of net-zero emissions, health care organizations will need to consider either purchasing GHG offsets or generating their own energy.
Purchasing carbon offsets or renewable energy credits can be an immediate solution to meeting GHG reduction targets, but this approach has limitations, including lack of general accreditation and offset quality, unknown future costs and unchanged dependence on fossil fuels. On the other hand, the time has never been better for health care systems to consider incorporating renewable energy generation into their energy portfolio.
The 2022 Inflation Reduction Act made significant changes in federal incentives for solar energy. Importantly, nonprofit organizations are now able to receive a direct payment in lieu of the federal renewable electricity production tax credit, which has been increased to 30% of project costs, with 10% bonuses for domestic manufacturing and projects in economically disadvantaged communities or those with significant fossil fuel economies.
As a result, solar energy projects can now often provide paybacks of seven years or fewer and internal rates of return in excess of 10%. Solar power installations are often warrantied for up to 20 years and can be expected to be operational for up to 30 years, making these projects one of the lowest risk long-term investments an organization can make.
Many organizations enter into power purchase agreements where a third party owns and operates a plant with the produced electricity being sold at a set long-term price. However, there are significant financial advantages to health systems owning their own power-generating assets. Any health facility with significant collocated real estate unlikely to be developed in the next 30 years would be well served to conduct a feasibility assessment of a solar-generating project. “Behind the meter” installations provide additional opportunities for emergency power redundancy and resiliency for long-term utility disruptions.
A new normal
Leaders in health care facilities and real estate are being asked to participate more broadly in health care’s decarbonization effort. Given the societal health benefits of this work, they should promote within their departments and organizations the idea that they are in the business of public health and wellness just as much as clinical staff. This responsibility is not just accomplished through the critical role of maintaining a safe and comfortable environment, but by taking initiative in reducing GHGs and other environmental pollutants.
‘CEGO’ is a plan within the plan
A climate action plan contains strategies that reduce emissions across all aspects of business operations. Reducing the impact of utilities is typically the starting point. University of Florida Health (UF Health) has followed an approach that progresses in complexity and cost and has steadily decreased its footprint by 24% over the past 10 years. It is composed of the following elements, which spell “CEGO”:
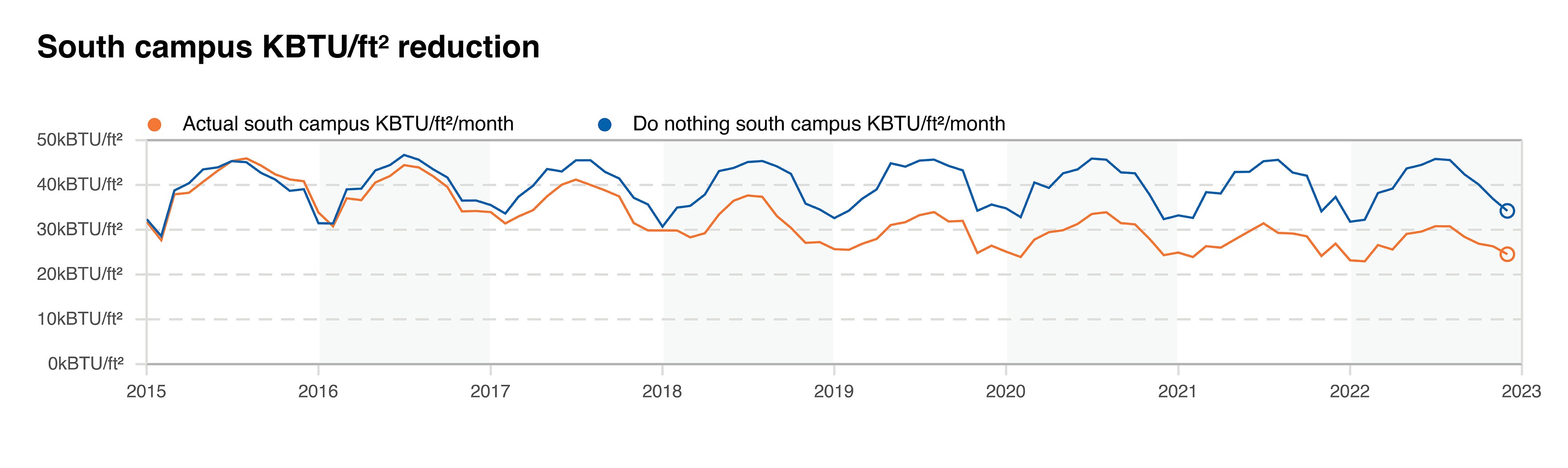
Conservation. Approximately 10% to 20% of gains come from making the best use of existing assets through conservation. UF Health accomplishes this through retrocommissioning, fault detection, insourcing controls and peer education. Its efforts have been homegrown from one curious project manager to a team of four full-time equivalent employees and several consultants in charge of driving savings, maintaining the gains and advancing digital tools.
Equipment. Every construction project is an opportunity to increase efficiency and transition to electric where appropriate. UF Health has taken an incremental and deliberate approach to progress its infrastructure with every capital project. Technology such as fan walls, high-performance variable air volume, energy recovery, LED lighting and series cooling coils is now ubiquitous. When it comes to electrification, several new medical office buildings are utilizing variable refrigerant flow heat-pump technology to operate fully on electric at 40% less cost than conventional counterparts.
Generation. To go deeper than a 30% to 50% reduction, a facility must start to produce its own power. UF Health has a combined heat and power plant that powers its south campus. When it comes to solar, it has a small visible array on its children’s hospital, and its local city-owned utility is in process of adding a 75-megawatt solar farm to the local grid that feeds several UF Health sites.
Offsets. Purchasing offsets — essentially investing in other people’s projects — is one of the last ways available to achieve net-zero emissions. UF Health has not yet found this to be important to its journey. It continues to have its own opportunities for savings and prefers to invest in projects under its control that have direct benefits for occupant comfort, patient safety and facility resiliency.
About this article
This is one of a series of monthly articles submitted by members of the American Society for Health Care Engineering’s Member Tools Task Force.
Kevin Gombotz, PE, is vice president of building energy solutions at Envinity Inc., State College, Pa. He can be reached at kgombotz@envinity.com.