Military health project focuses on resiliency

The William Beaumont Army Medical Center in El Paso, Texas, is designed for resiliency under evidence-based design principles.
Photograph by Dan Schwalm, HDR
Over the past decade, man-made and natural events have emphasized the need for greater resiliency in individual facilities as well as more resilient buildings overall. This is especially true in the world of health care facilities. However, this term is not always well understood or correctly applied.
Resiliency is broadly applied by the architecture profession, causing it to take on many meanings across a wide array of planning and design solutions. If the design community is to progress and improve hospital resilience, it must coalesce around a clear concept of resiliency in the context of health care design and identify its key domains.
Having a clear concept for resiliency is especially critical for military defense, where expectations for continued service are higher and the range of threats broader. While this may pose a challenge to many public and private health organizations as a first-time consideration, one of the more impressive aspects of the Military Health System (MHS) is that it has tackled the concept of robust and resilient hospitals at least for the better part of a decade.
This is not to undercut other efforts in health care design resiliency, but to underscore that resiliency has been at the core of the MHS’ ethos for many years, fundamentally to serve as the last line of defense in life preservation during all types of disasters, including natural, chemical, biological or war-related.
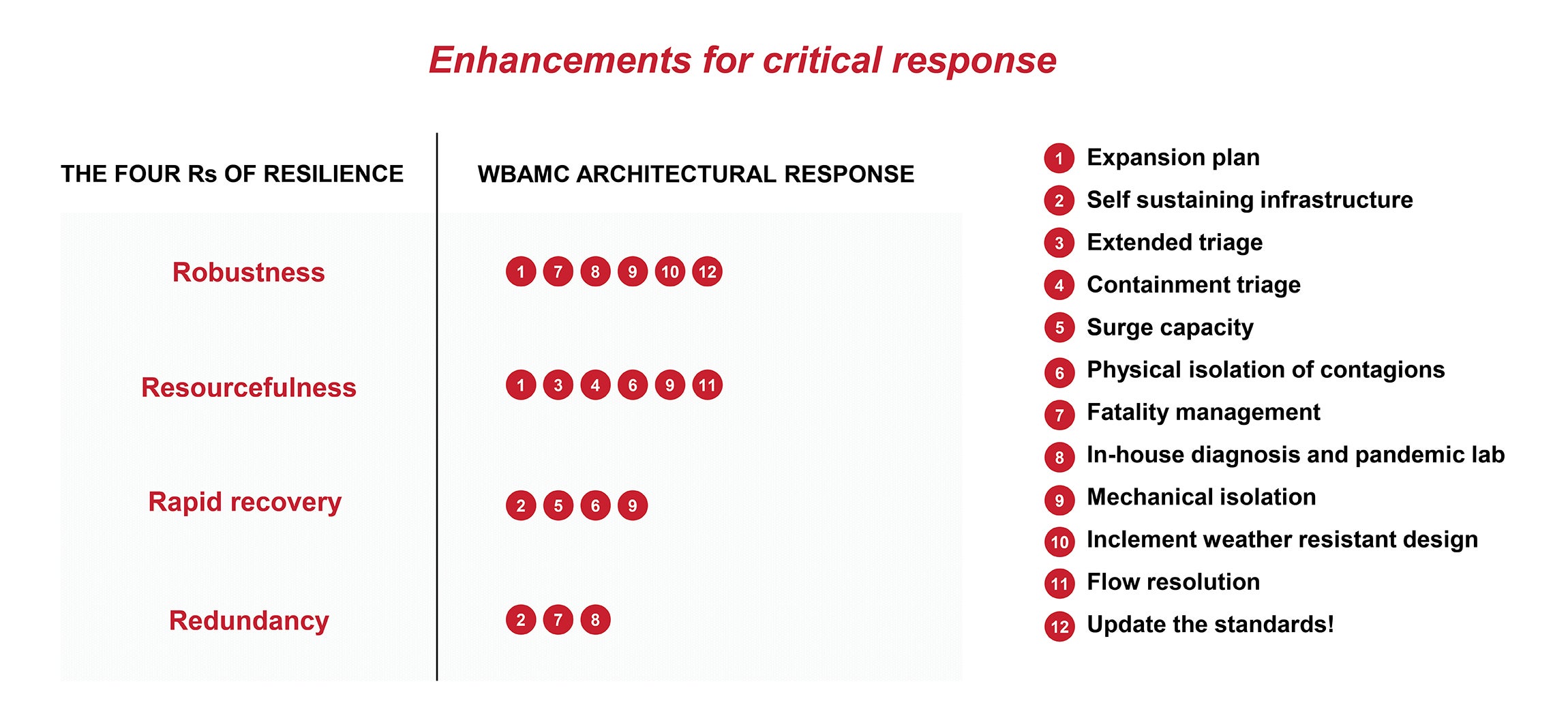
The Department of Defense (DOD) recognized a need for resilience in its core infrastructure and attempted to define the components of building resiliency in 2009 when it adopted the “four Rs” of resiliency as part of its Whole Building Design Guide (WBDG). The four Rs were adapted from the National Association of Insurance Commissioners’ resilience research, which characterized resiliency by robustness, resourcefulness, rapid recovery and redundancy.
The application of the four Rs is intended to be broad and to cover many types of buildings and civil infrastructure. This makes interpreting its application to the hospital setting challenging and leaves health care facility designers without a clear roadmap. Despite these hurdles, the four Rs formed the foundation of a 10-year pursuit to build the MHS’ first fully robust and resilient hospital under the WBDG, the William Beaumont Army Medical Center (WBAMC).
Resilient military campus
Opened in 2021, the current WBAMC in El Paso, Texas, is the largest military medical facility in the Western Region Medical Command and the boldest and most sophisticated health project undertaken by the DOD.
Designed for resiliency under evidence-based design principles, the world-class medical center’s core mission is to provide care for active-duty military and their eligible family members as a state-of-the-art Level II trauma center.
WBAMC was designed under the WBDG’s resiliency parameters to withstand mass casualty events of all kinds and to provide patient containment as needed, while also being able to maintain and expand medical capacity in response to sudden increases in patient demand.
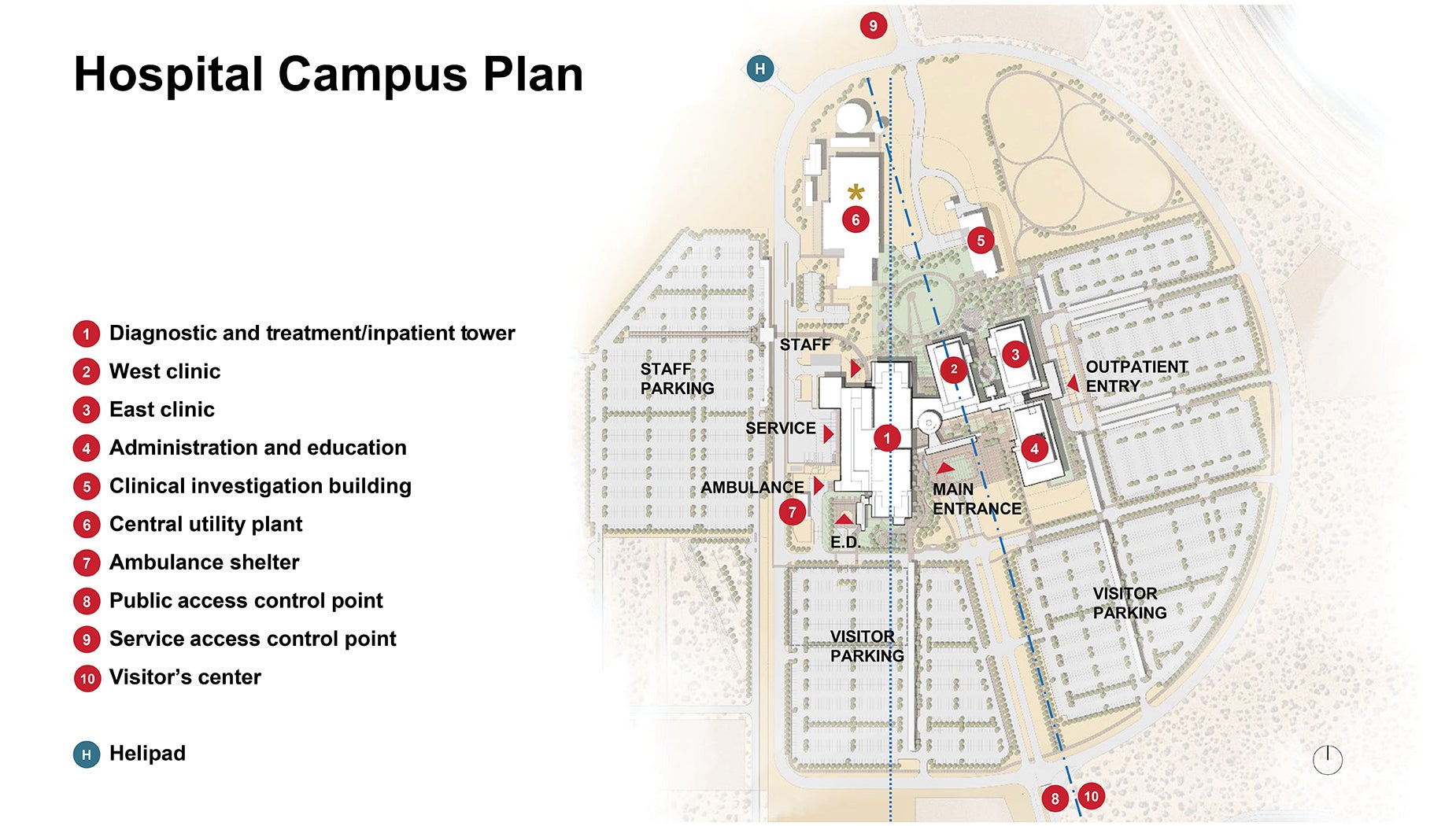
The 1,130,000-square-foot medical center forms a campus within a 260-acre site, located in the Chihuahuan desert near the West Texas city of El Paso. Embracing desert conditions and a barren ecosystem where architectural context is absent, the project is integrated into the environment’s rich natural surroundings: the distinctive hillock vegetation and the Franklin Mountains. The exterior expressions are drawn from these cultural sources and other climatic and functional considerations.
The campus is comprised of five main buildings, five supporting buildings and one helipad. The design has flexible and adaptable components, featuring solutions that solve for both long-term resiliency and emergent responses.
Applying the four Rs
The DOD adopted the four Rs as part of the WBDG in 2009, which coincided with the early design phases of WBAMC. This left the design team at a distinct disadvantage but also provided an unprecedented opportunity to pioneer the deployment of the four Rs in the health care setting.
The team’s interpretation of the four Rs was to focus on how the building could enhance or protect critical operations in the face of a disaster or threat.
The following critical outcomes were used to bind the four Rs together in an application-learning-refinement cycle of resilience planning: First, safety of inhabitants is achieved through “robustness and resourcefulness.” Preparedness for a rapid influx of patients is accomplished via “resourcefulness and rapid recovery.” Continuity of service for existing and new acute patients (meaning, the system is flexible enough to avoid being overwhelmed) is reached through “rapid recovery and redundancy,” and, finally, recovery and learning is realized after “redundancy” and feeds back into “robustness.”
Thus, the four Rs apply to the WBAMC project in the following ways:
Robustness. This supports the entire continuum of care from inception to end of life, ensuring holistic patient care and environmental protection within the medical center with full in-house services and infrastructure redundancy. WBAMC siting brings a purposeful geometric order to this barren desert site.
The north-south alignment of the building components are arranged to shelter the outdoor spaces from the desert’s strong westerly winds and violent sandstorms. The facades protect the narrowly proportioned courtyards from the high desert sun angles. A planned 15-degree rotation between buildings aligns the main circulation spine parallel to the historically significant Butterfield Trail.
Resourcefulness. This is represented through an understanding of site constraints, paired with knowledge of governing guidelines and MHS requirements, design innovation and creativity, resulting in maximizing the resources of the building environment. As a result, WBAMC presents extended triage, physical isolation possibilities and clean flow resolution through long-term and emergent responses, as well as maximized patient care areas with a site-responsible infrastructure.
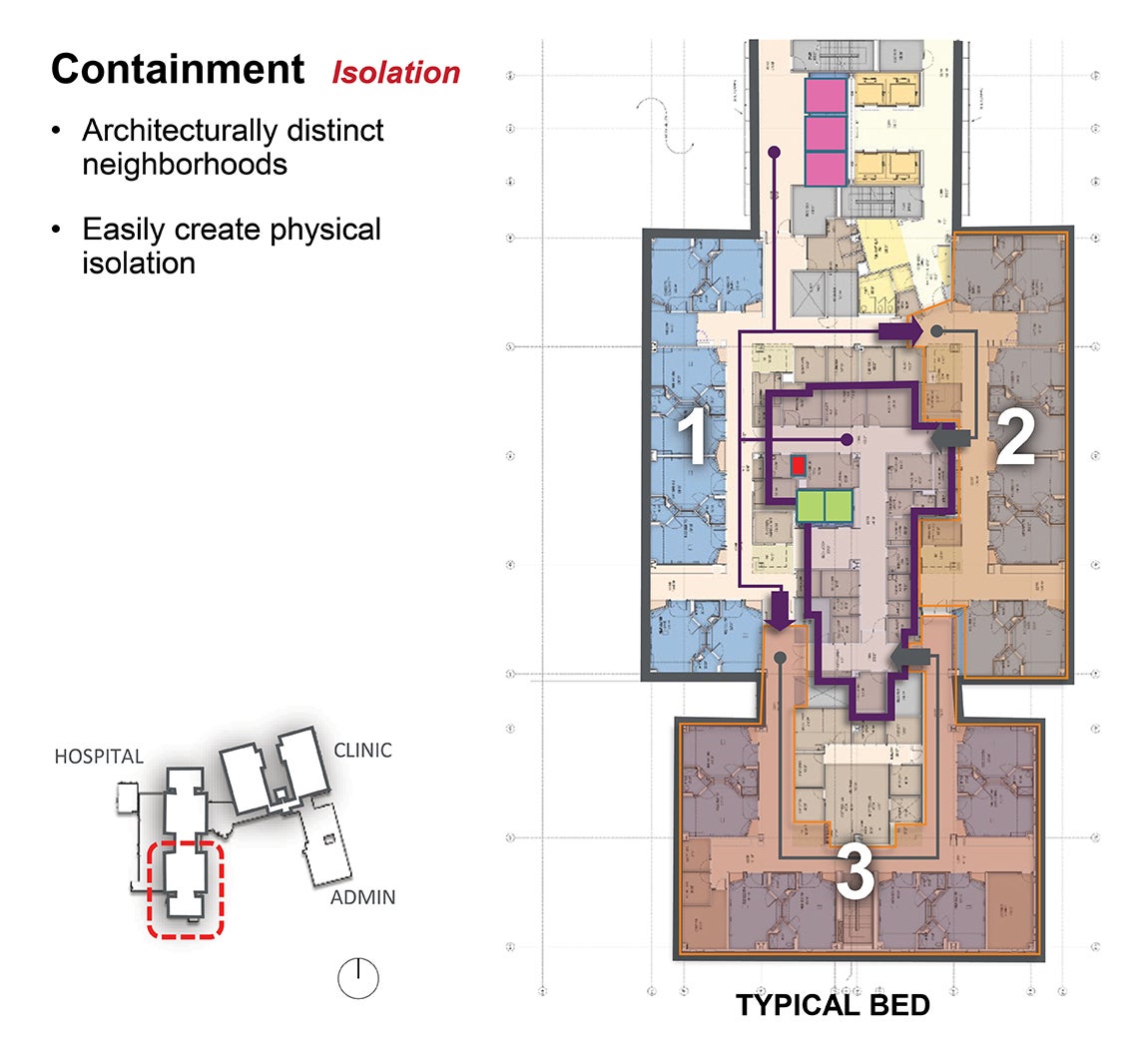
Rapid recovery. This is provided by an expanded surge capacity, resolved by several design features, including architecturally distinct neighborhoods that easily create physical isolation and provide compartmentalized care pods. The building blocking and stacking allows the facility to react quickly to change in space functions without compromising isolation or containment needs.
Redundancy. This is mainly achieved by an N+1 building systems design with self-sustained mechanical systems, protected infrastructure and an enhanced service yard. The yard serves extended fatality management and redundant materials handling. To help ensure isolation or containment, the pneumatic and chute materials handling systems for recycling, trash and linens play a key role, routing compromised materials away from human exposure.
Long-term and emergent resiliency
Twelve health care planning strategies and concepts enhanced the WBAMC design solution for critical response by utilizing the DOD resiliency framework under the four Rs. These are split between long-term and emergent resiliency responses.
Long-term resiliency. To provide long-term resiliency, the building design resolves expansion needs, systems redundancy and protection from special threats. Its planning strategies and concepts include:
- Expansion plan. Expansion capabilities are provided at the campus level to meet the 25% building-required expansion target. The organization and building expression of WBAMC is structured around a main circulation spine that permits simultaneous radial growth of critical and independent programmatic components, including diagnostic, treatment, inpatient care, surgical functions, administration, education and outpatient programs. This organization and expansion strategy maintains the integrity of all flows, wayfinding, building expression, purity of adjacencies and departmental planning, along with the truthfulness of the block-and-stack plan.
- Self-sustaining infrastructure. While most hospitals are designed to recover quickly from normal events such as power outages, water main breaks or natural disasters, WBAMC is designed to support continuous emergency services during unique events, such as those encountered during times of war. Redundancy provisions are in place for a continuous supply of power, water, medical gas, communications and all critical infrastructure during the range of possible disruptive events. This includes 96 hours of on-site power generation, continuous freshwater production and four days of medical gas supply.
In addition, the Unified Facilities Criteria (UFC) antiterrorism and force protection measures design guides are applied to the building envelope and structural system to protect against blast, bombings, civil unrest, vehicle ramming, ballistics, forced entry and complex attacks. The design also considers special threats like cyberattacks and extreme weather.
Emergent resiliency. This is accomplished through two distinct but complementary strategies: to ensure support during mass casualty situations and/or to support biological or chemical containment while enabling a comprehensive response to the needs of patient populations under either scenario. Its planning strategies and concepts include:
- Extended triage. During mass casualty events, triage is extended out to tents in the visitor parking lot and ambulance shelter adjacent to the emergency department (ED). This extends patient treatment space, saving the hospital for the most critical patients and keeping the system from becoming overwhelmed when patients begin showing up in rapid waves.
- Containment triage. There are two areas on campus designated for large volume pandemic or chemical triaging in addition to the compartmentalized ED and the fever and upper respiratory clinic building. Both areas have dedicated, mechanically isolated access points to the medical center that prevent further impact on the rest of the hospital.
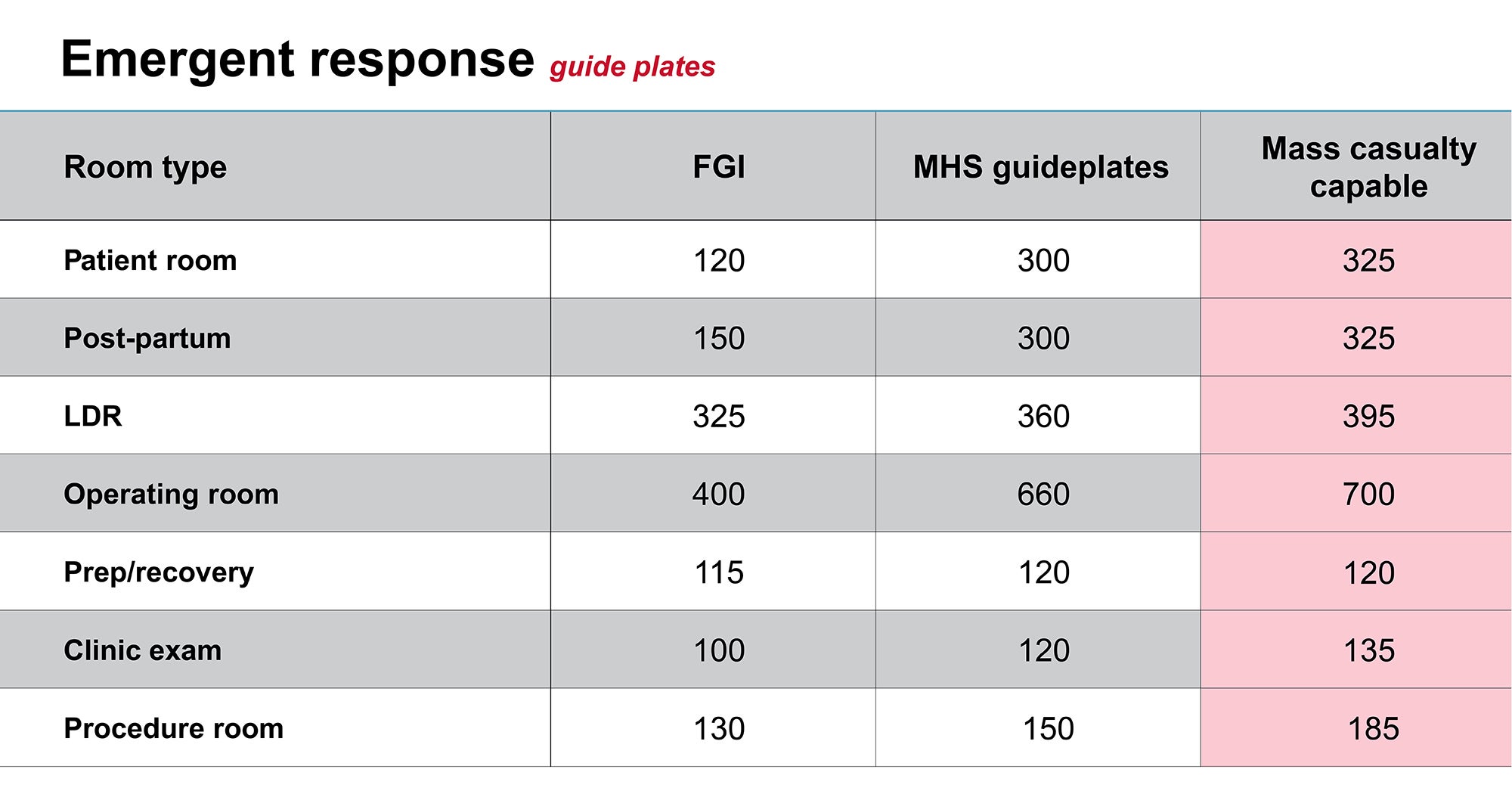
- Surge capacity. The hospital is designed to maintain and expand medical capacity while responding to significant increases in patient demand. This required the team to design care spaces to be used in untraditional ways. The team designated flexible spaces as emergency response space (ERS) and designed private patient rooms large enough to adapt into semi-private rooms; created oversized clinic exam space so it can be used as step-down or low-acuity inpatient space (preserving inpatient beds for the most critical patients); designed minor procedure rooms to higher requirements to be used as overflow operating rooms; and used academic simulation space as additional operable procedure spaces.
- Physical isolation of contagions. Physical and mechanical isolation of zones within the hospital ensure that airborne pathogens will not spread beyond designated areas. This intervention starts at the main entry points of the facility after external triage/treatment.
Two entries are designated for infectious patients: the fever and upper respiratory clinic building and an isolation pod within the ED. If continued treatment or observation is needed, patients are admitted and taken up dedicated infectious elevators to the inpatient unit where care is broken into smaller physically isolated care pods of eight patient rooms.
Each wing of the bed tower has three similar isolated care pods that can function independently, for a total of 24 beds in each mechanically isolated wing. Dedicated clean elevators allow for movement of staff in a safe zone where the donning of personal protective equipment (PPE) can occur before entering one of the three eight-room care pods.
Soiled linen and trash are removed via pneumatic chutes, further protecting care providers from potential contamination.
- Fatality management. During a surge in a community, end-of-life management inclusive of morgues, funeral homes, crematoriums and cemeteries may not have the capacity to carry out timely transfer from hospitals. Thus, the design of the service yard at WBAMC allows ample space for long-term refrigerated morgue trailers, supply storage including body bags and PPE, disposition of remains and family reunification. Most hospitals have limited morgue capacity and may become overwhelmed quickly during a surge in pandemic-related deaths.
- In-house diagnosis and pandemic lab. Access to immediate laboratory diagnosis and results is provided by a biosafety level three (BSL-3) laboratory within the diagnostic and treatment podium located vertically adjacent to the ED area, available for point-of-care testing at all triage and patient areas, several satellite specimen collection points and the pneumatic tube system.
- Mechanical isolation. When responding to pandemics or other containment situations, mechanical compartmentalization of the hospital becomes a primary commodity that ensures uninterrupted service to non-infected medical patients and safety to hospital staff. Further, delineating space for containment that is mechanically isolated can save PPE resources, which tend to become valuable commodities during pandemics. WBAMC is mechanically split into multiple care zones, including the fever and upper respiratory clinic building, the ED, the BSL-3 lab, each individual wing of the inpatient tower and a BSL-2 lab in the clinical investigation building.
- Inclement weather. Resistance to extreme weather events is resolved through rainscreen systems, passive solar shading strategies and concepts reducing solar heat gain, minimizing glare and lowering energy consumption, and through sand-resisting envelope materiality.
- Flow resolution. Key drivers for the block-and-stack resolution — beyond solving for continuity of services, efficiency, patient care, wayfinding, travel distances, operational and functional programming, and the seven flows of health care — include solving for the military mission, the inclusion of the graduate medical education component and the impact of mass casualty and containment needs.

The design also considers special threats like cyberattacks and extreme weather conditions.
Image courtesy of HDR
This perspective created a solution that extends surgical services across all buildings. Similarly, other lines of services were linked across bridge components such as women’s services and mental health. The main spine and the service floor are fundamental for campus resiliency.
- Updated standards for surge capacity. As part of the ERS, the team sought to provide mass casualty capable rooms that went beyond the standard room sizes to effectively offset patient surges. This was attained by designing spaces that could readily double in capacity and adaptively use clinic and procedural spaces in unique ways.
The design team’s ultimate mission was to achieve continuous improvement of DOD building standards by not exceeding the guidelines maximum program deviation while still setting a standard for future resilient-driven MHS projects.
Pioneering program design
The design of the William Beaumont Army Medical Center not only fulfills its mission but delivers exceptional resiliency and disaster management capability.
It creates the ability to maintain and expand medical capacity in response to sudden increases in patient demand, with nimbleness and comprehensive preparedness, by implementing the four Rs and with a pioneering program design.
Critical adjacencies aid resiliency
While much focus is spent on how site, mechanical systems and room design can build resiliency for hospitals, how building design can bridge operational efficiency into the resiliency equation should be of equal importance. When designing large, multifaceted hospital campuses, it is important to consider strategic adjacencies across buildings that allow resources and staff to be shared quickly and seamlessly.
Even under normal circumstances, staffing shortages afflict many health systems across the country, if not the entire modern world. By connecting the outpatient realm with literal or figurative bridges back to similarly specialized inpatient care areas, staff can more effectively administer care between two cost centers, thus providing the benefits of their specialization to patients at any point in their care journey and on any given day.
Further to this point, more complicated procedures are being pushed to outpatient centers for cost or reimbursement reasons, putting an extra burden on staff and physical resources, especially when these procedures involve high-risk patients. By exploiting the same physical connections provided for staff between the hospital and outpatient clinics, these procedures will have the benefit of resources and potentially life-saving support from the main hospital.
About this article
This feature is one of a series of articles published by Health Facilities Management in partnership with the American College of Healthcare Architects.
Susana A. Erpestad, AIA, ACHA, EDAC, is the global director of federal architecture at HDR Inc. and Matthew Suarez, AIA, ACHA, EDAC, is a health planning principal at HDR. They can be reached at susana.erpestad@hdrinc.com and matthew.suarez@hdrinc.com.