Simulation modeling to improve clinic layouts

The integration of discrete event simulation during the planning process enabled the adaptive reuse of a mall reimagined as an outpatient clinic with 12 departments.
Image by BSA LifeStructures
A design professional’s ultimate responsibility is to advise clients on their capital spending. Over recent years, several tools have emerged to eliminate uncertainty in the built environment before the design takes physical form.
One such tool is discrete event simulation (DES), which provides a cost-effective method to evaluate and inform future design decisions for capacity estimation, policy impact, patient scheduling, patient wait times or process modeling. DES evaluates the effects of multiple variables, alternative solutions and decisions on optimal scenarios. The extensive use of DES in health care emerges from its complex, unpredictable and variable nature.
Over the past 40 years, DES models have been growing in popularity and acceptance by health care administrators as practical tools for resource allocations that improve patient flow and satisfaction.
Efficient operations
Given the complexity of outpatient facility operations, DES is considered an effective tool to evaluate resource pooling, performance outcomes, resource utilization, capacity and turnaround times across different situations. A growing number of studies have employed DES to resolve issues such as patient wait time for providers or clinic rooms by evaluating alternatives for patient scheduling, performance measures or resource allocations.
Pooling existing resources fulfills patient demands and yields operational progress in resource planning. Additionally, considering the staff shortages in the health care field, DES provides opportunities for exploring staff reduction for efficient health care operations.
Over the past decade, there has been an increasing demand for outpatient services. According to a 2019 Health Care Cost Institute study, outpatient services increased from 11.1% in 2009 to 12.9% in 2017. The increased outpatient volume has boosted pressure to reduce operational costs and improve resource utilization for outpatient health care services.
The delivery and management of multidepartment outpatient facilities are complicated. These facilities include multiple stakeholder processes, including physicians, nurses, nurse assistants and patients.
Further, appointment types, availability of resources and patient arrival times impact the outpatient delivery systems. Therefore, having a logical decision-making process to achieve efficient outcomes, such as improved waiting time or resource utilization, may be challenging in these settings.
Clinic case study
The following case study describes the integration of DES during the planning process for the adaptive reuse of a mall reimagined as an outpatient clinic with 12 departments, including primary care, pediatrics, obstetrics-gynecology and neurological.
The city and the health care system’s dual ownership of the project created a synergic partnership for improved health through a new wellness and recreation campus of approximately 400,000 square feet. Planning and design teams identified architectural precedents for innovative approaches that improve health, wellness and optimal operational outputs.
To achieve patient-centered outcomes, designers sought to enhance wayfinding experiences and convenient parking access for acute or chronic illness patients. Designing a public concourse was a patient-centered innovation that aimed to improve wayfinding, visibility, patient engagement and flexibility for future adaptation. The pod-based onstage/offstage departmental layouts aimed to increase caregivers’ face-to-face communication and improve team dynamics.
Careful planning of exam rooms, staff rooms or equipment resources is integral to effective and efficient care delivery for outpatient clinics. Nevertheless, the variability in the registration, check-in, intake or exam process makes resource planning complex. Typically, facilities managers evaluate resource planning from a narrow perspective that comes from years of operating as stand-alone entities versus when consolidation occurs.
Many cost estimates depend on fixed resources independent of the patient arrival schedule. These include exam rooms, staff or equipment that can be modeled as a practical means of better interpreting the interactions between processes, and the physical environment and its impact on operations.
In this case study, the health care organization expressed interest in measuring the effects of a decentralized to a centralized registration system that influenced space allocation. It also wanted to evaluate if the proposed number of exam rooms per department is adequate for optimum future performance and potential patient volume growth. Further, the design team explored how staffing or resource allocation may affect patients’ wait time.
The DES model was built in FlexSIM 2021 by FlexSim Software Products Inc., Orem, Utah, with the design of a conceptual model representing typical operations for each of the 12 departments. A comprehensive analysis was performed on data from more than 170,000 appointments between July 2020 to June 2021 (n = 176,286). As part of the study limitation, the design team acknowledged that the patient volume might have been affected by the COVID-19 pandemic.
Fundamental elements of DES in health care include patient flows through the system, arrival rates, location resources, equipment resources, staffing resources and service time. Location resources were based on the proposed clinic floor plan undergoing the planning and design process. For example, each exam room, registration desk or kiosk was considered a location resource.
The base model outputs were validated and verified with real-world data. Staffing resources were estimated based on the organizational proposed staffing schedule per department. Administrative and clinical staff per department verified that process logic connected all the model elements. Performance measures included patient waiting for a provider, room utilization rate or waiting for an exam room.
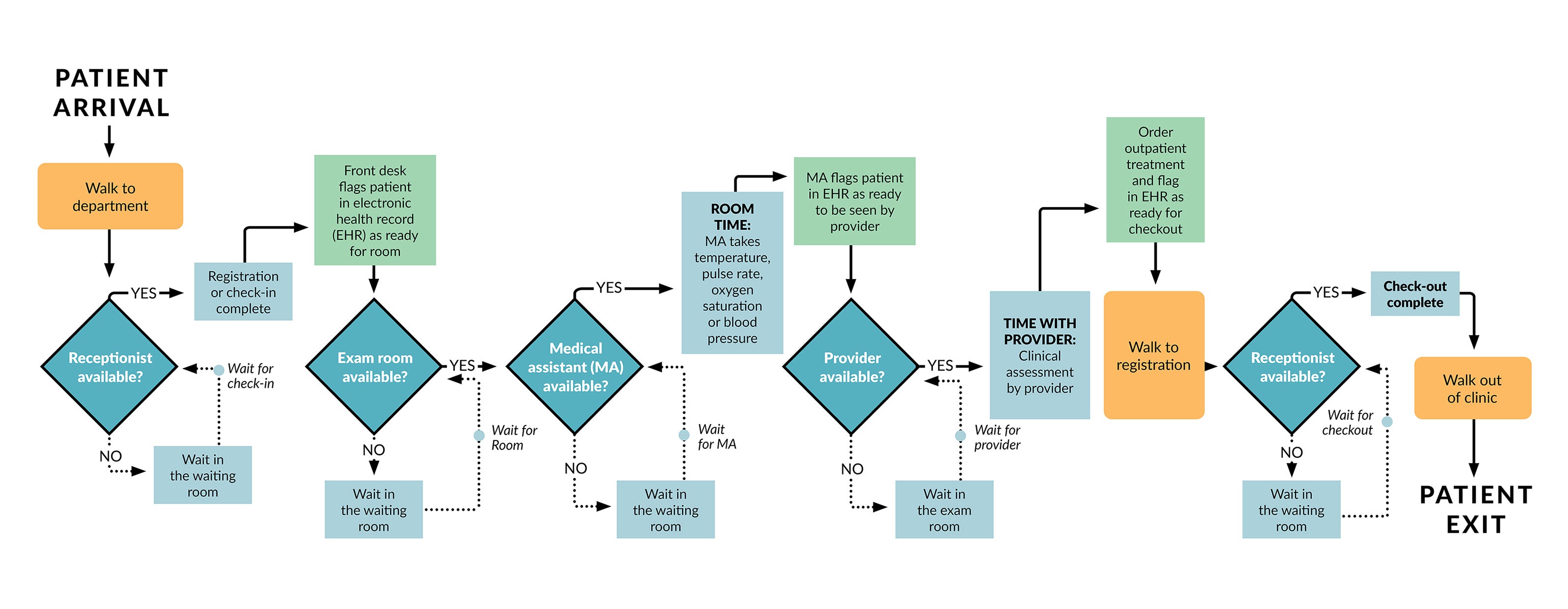
Typical patient flow in the clinic’s primary care departments.
Image by BSA LifeStructures
The design team mapped the flow of patients from the actual stages of the system. The graphic above displays the patient’s steps for routine primary care. Initially, patients enter the building from the main entry point and walk toward the concourse and the department of interest. Patients stop at the registration desk to complete registration or check-in and await their appointment.
Afterward, a medical assistant (MA) or a licensed practical nurse (LPN) escorts the patient to an exam room. The clinic’s historical data identifies this period as the “room time,” in which the MA or LPN collects vitals and necessary information and reports the results to the electronic health record and physician.
Patients remain in the exam room until the physician is available and enters the exam room, described as “the time with the provider.” In addition to the time with patients, physicians are required to complete paperwork and documentation following their appointment.
Sometimes, documentation overlaps MA-patient periods or when no patients are in the clinic. The model assumes that if a patient is ready and waiting in an exam room, the physician prioritizes seeing the patient rather than completing the documentation process. Finally, MAs escort patients to the check-out desk from where they leave the clinic.
The model considered all these details to ensure accuracy in the system representation. To address the first issue, the design team modeled and pooled the registration desk for the primary care departments on the east and west sides of the building. Then, operational outcomes were compared to the original state, including staff utilization and the registration wait time. In the current state scenario, the planners had assigned each department a registration area where patients complete registration, check-in and check-out.
This decision stemmed from user group conversations across departments suggesting this implication would be a viable option for this department. Staff from the other departments mentioned that merging the registration desks with other departments may be problematic for specific patient demographics or types. Clinicians and administrative staff also perceived that primary care patients could benefit from utilizing kiosks for check-in, completing registration or check-out. The simulation scenario includes six kiosks on the west and two on the east side of the clinics, presuming that 20% of patients will use kiosks for check-in or registration.
Findings established that a centralized registration system with pooled staffing resources improved staff utilization from 31.8% to 49.4%. The result showed that such alterations did not substantially affect patient wait for registration or average registration staff utilization (an increase from 33.8% to 49.5%). DES also explored the impact of directing patient check-in or check-out flow to kiosks for targeted departments on patient length of stay and wait time. The model showed that kiosk integration reduces wait time and the physician-to-administration staff ratio, thus saving costs.

The FlexSIM platform provided a 3D virtual interface for enhanced communication.
Image by BSA LifeStructures
The purposeful addition of a flexible exam/counseling room for peak patient volumes reduced patient wait for exam rooms in targeted primary care departments. For example, for one of these departments, the wait for the exam room reduced from 44.7% to 20.1% during high-peak patient volumes. Nevertheless, during average patient volume days, the department worked efficiently with the proposed number of exam rooms. This finding implies the importance of flexible exam-consult rooms as alternatives for patient treatment during high-volume patient flows.
The team explored the effects of transforming several underutilized exam rooms into telehealth rooms or sub-department waiting through an alternative scenario. The intent was to accommodate intentionally designed telehealth rooms directed toward its increasing demand for outpatient clinics.
Additionally, recent literature suggests the need for dedicated telehealth rooms for clinic departments. Further, clinics need intentionally designed and dedicated telehealth rooms to accommodate appropriate lighting systems, angles or colors. These rooms need high-quality speaker systems, video cameras and monitors to ensure reliable and effective communication during telehealth visits.
Finally, ensuring patient privacy through audio and visual qualities in telehealth rooms is crucial for a successful design. The simulation model effectively explored the impact of underutilized exam room reductions on patient wait times or exam room utilization. The scenario model showed that such resource alterations would not substantially impact the exam room utilization for such departments.
For example, the exam room utilization for the pediatrics department increased from 24% to 29% after reducing its number of exam rooms from 24 to 20. This finding was critical and an excellent opportunity for improving the patient experience.
Studies suggest that separating the waiting areas for pediatric patients from adults creates playful experiences, offers a sense of security for children, encourages social interactions, and improves patient and family satisfaction. Further, integrating positive distractions in clinical settings enhances pediatric patients’ well-being and contributes to holding their attention during wait times. Thus, DES was an effective tool, suggesting that interior designers and planners create a lively and pediatric-friendly waiting room that reduces the perception of waiting for patients and families through a comfortable and engaging experience.
The findings from this study pointed out that pooling resources was an effective strategy for improving space and staff utilization. Centralized registration desks for the primary care departments improved staffing and space resource management. Additionally, altering several underutilized exam rooms into a pooled telehealth room resource improved room utilization and exam room availability across departments.

The proposed layout of the clinic and the relationship between the clinic’s different departments, including those that were not part of the simulation.
Image by BSA LifeStructures and RSP
The project showed that involving medical and management staff during the simulation development ensured that the model represents a realistic situation for the future clinic. It also benefited from defining reasonable and achievable strategies for pooled resources across the departments. Beyond this, the simulation model’s graphic and video outputs enhanced stakeholders’ communication and decision-making and facilitated model validation.
The limitation of this case study mainly relates to extrapolating the findings from this multiclinic facility to other contexts or practices. During the interviews, clinicians described how they sometimes forgot to record appointment details in the electronic health record system. Consequently, data validation and interpretation were a significant challenge, as many of the historical patient data needed further evaluation and outlier removal. Nevertheless, the results from this case study are transferrable to other organizations with similar flow processes or patient volumes.
An effective tool
The application of DES analysis was an effective tool in architecture planning for evaluating the impact of design alternatives on performance-driven outcomes for the future state of the outpatient clinic. Additionally, DES provided an experimental setting to test design scenarios and improved architect-owner communication.
This case study allows managers to offer optimal staffing and clinical spaces and encourages resource pooling in multiclinic facilities to reduce costs and staff needs through simulation modeling.
The validity of predictive simulation models needs to be assessed through future clinical and operational data or site observations. Cultural, social, behavioral and psychological dimensions may affect the projections.
For example, in this study, the percentage of the patient population using the kiosks for registration depends on demographics or comfort levels using technology interfaces. Existing literature recommends employing post-occupancy evaluations to triangulate and verify the simulation findings in real-life work environments.
DES was an effective tool to propose programming alterations to the clinic environment. These modifications aimed to accommodate the growing integration of technology and environmental features that improve the waiting experience relative to the visitor’s well-being. The emerging tools provide data for health care organizations to make informed decisions, but they are still complicated and resource intensive.
The design team invites a future where quantitative and qualitative solutions are considered from a single workflow and are more intuitive.
Adaptive reuse helps organizations economically decentralize operations
Transforming social, political and economic factors impact the design and modalities of health care systems. Despite the prevalence of virtual health care delivery methods, health care systems require physical environments to provide comprehensive patient care.
Health care real estate expenditures lessen financial resources that must be invested to deliver health and medical services to patients. One approach to saving capital is recognized as “adaptive reuse.”
Adaptive reuse is the practice of detecting, attaining, renovating and operationalizing a building or a structure for another function. It encourages communities to maintain or recapture endurance, improve aesthetic qualities, revive businesses and conserve natural resources.
Health care systems across the U.S. are expanding their service from centralized medical centers to new patient communities. These contemporary trends impose a variety of new opportunities for the adaptive reuse of malls into health care centers.
There is a growing trend for hospital systems to develop and reuse malls primarily established in diverse neighborhoods. This implication maintains capital, saves time, conserves resources and enhances patient access to care.
Further, malls generally provide conveniently accessible and adequate parking spaces near major highways. Such transitions benefit existing retail tenants and provide meaningful access to health care services in the community.
About this article
This feature is one of a series of articles published by Health Facilities Management in partnership with the American College of Healthcare Architects.
Timothy J. Spence, AIA, FACHA, is president, and Zahra Zamani, Ph.D., EDAC, LSSYB, is senior design researcher at BSA LifeStructures. They can be reached at tspence@bsalifestructures.com and zzamani@bsalifestructures.com.




