COVID and social comparison: Making sense of the unknown
When faced with a potentially important and unknown experience, people seek out objective information so they can understand, cope and guide their own behavior through the situation. However, there are cases when objective information is scarce, and people need to find other sources of information. One way people do this is through “social comparison.”
Social comparison occurs when one purposefully compares oneself with someone else on an attribute or thing that is important to them. The results of this comparison help the person who did the comparing get a better understanding of themselves and the current situation.
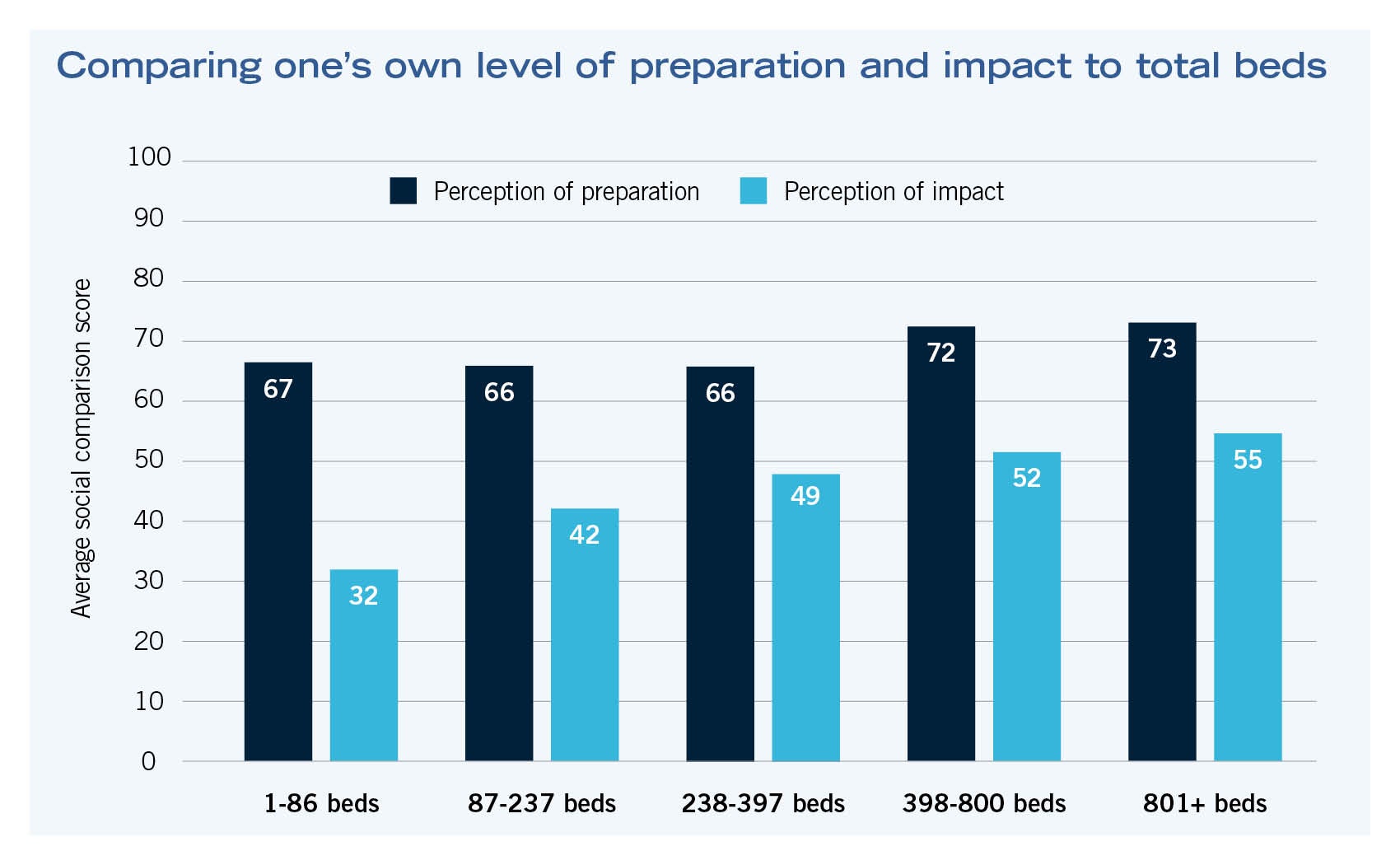
The COVID Response Tactics Sharing (CRTS) survey project asked respondents to engage in two social comparisons, one where they compared how much they thought they prepared, as compared to others living in different areas of the country, and then another, where they compared how impacted by the crisis they think their local health care facility was compared to others across the country. The chart at the bottom of this page illustrates the average scores for each of the different member roles. Even though there were slight differences in the scores, the differences were not large enough to be systematically different. As expected, surge preparation and surge impact scores were related, but surge impact scores were, on average, lower than surge preparation scores. Given that this is a nationwide sample, and people’s perceptions of how much they prepared and how much they felt they were impacted by patient surge could be related to several factors, tests were conducted that compared hospital setting (urban, suburban, rural) and numbers of inpatient beds as well as numbers of long-term care beds.
Interestingly, respondents from rural settings, on average, rated their surge impact experience significantly lower (20 points) than respondents from suburban or urban facilities. This same relationship was not found for respondents’ perceptions of surge preparation. Analyses also found that the number of inpatient beds was positively related to impact perception scores (but, again, not surge preparation perception scores). Respondents from facilities with larger numbers of inpatient beds perceived their facility to be more impacted by patient surge than facilities with lower numbers of beds.
Because the field is still living in the COVID crisis, and a full understanding of this crisis will not occur until it has come out the other side, these findings provide some additional insight as to how peers in facilities management perceived their own surge preparation efforts and their unique perceptions of their own surge impact. These results fit into what has been learned about COVID-19’s patterns of transmission so far. However, true understanding of the COVID crisis will only occur after the pandemic is under control, and data patterns fully analyzed.