A review of common hospital utility risks

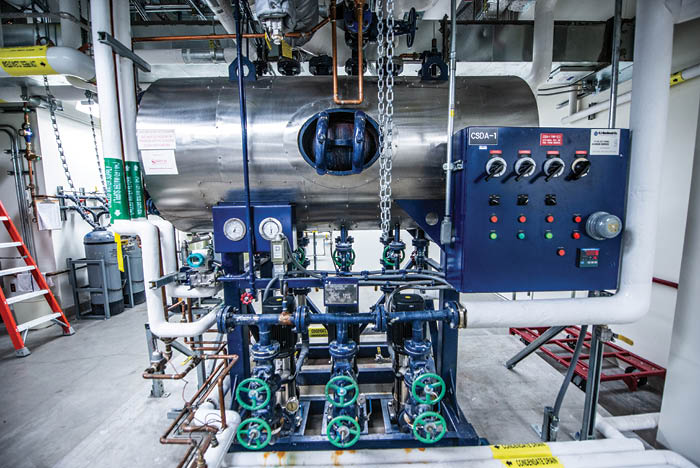
Multiple-boiler systems can provide spare capacity for scheduled maintenance downtime or the unexpected failure of a single boiler.
Health care facilities are served by numerous utility infrastructure systems and their related equipment. Among these are the heating, ventilation, air conditioning and refrigeration (HVACR) systems; plumbing systems (including water, waste and piped gases); and the electrical systems (both normal power and the essential electrical system).
This includes the building automation and control systems, information technology and communications systems, pneumatic tube systems, fire alarm and fire suppression systems, and even clinical technology systems and equipment.
Risk minimization concepts and strategies that apply to these systems should be reviewed periodically to ensure safe and efficient facilities operations.
HVACR systems
Ventilation systems provide appropriate pressure relationships, air exchange rates, filtration efficiencies, temperature and humidity in critical care areas designed to control airborne contaminants. Requirements pertaining to air-exchange rates and filtration efficiencies are generally less intensive in noncritical care areas.
The requirements are mandated by NFPA 99, Health Care Facilities Code, along with the corresponding referenced editions of the Facility Guidelines Institute’s FGI Guidelines and ANSI/ASHRAE/ASHE Standard 170, Ventilation of Health Care Facilities, or the applicable state design requirements if they are more stringent.
The “ASHRAE Position Document on Airborne Infectious Diseases” offers help in responding to problematic conditions.
Operating room (OR) humidity excursions outside desired parameters can have negative ramifications, according to the Association for Professionals in Infection Control and Epidemiology’s 2015 “APIC Infection Preventionists Guide to the OR,” which states, “… Low and high humidity can impair the accuracy of measurements taken using electrical conductivity. Over a long period of time, low humidity can deteriorate the wrap used on sterile items and compromise the sterility …” This document also contains a proposed set of questions that can be useful in conducting the APIC guide’s “Risk Assessment for Lower OR Humidity Levels.”
The Anesthesia Patient Safety Foundation’s June 2019 APSF Newsletter article on “Humidity Levels in ORs,” states: “Whenever the RH of a room extends beyond the approved limits, a risk assessment (RA) of the event should be conducted to ensure there is no adverse effect. A multidisciplinary group including physicians, surgical staff, infection control, OR management, clinical engineering, supply chain and facilities engineering personnel should participate in the RA. A review of the event, and its impact on environmental or operational conditions, should be evaluated and documented. The RA becomes the evidence that the operational breach had no negative safety consequence, and may also be used as a basis for future performance evaluations. This RA documentation also serves as a record of performance when authorities having jurisdiction perform inspections.”
Because ORs are required to have positive ventilation air pressure with respect to surrounding spaces, it is important to have the capability of validating compliance and similarly for each step down in pressure relationship. A common source of pressure relationship breaches is overuse of the OR doors during surgery, which may be corrected with better OR traffic control.
HVACR failures can involve a boiler, a chiller, an air-handling unit, a heat exchanger, an exhaust fan or any other single item of equipment, including perhaps a major portion of a building automation system.
The failure also can include all mechanical equipment powered by a failed electrical motor control center or all mechanical equipment powered by an electrical unit substation. HVAC system risks can even include unwanted failures of equipment or filters.
It is important to maintain current, accurate on-site documentation of equipment power sources and the areas covered by related groups of mechanical equipment in order to allow more rapid response to such cascading failures.
Different items of HVACR equipment plus emergency generators can utilize gases (carbon monoxide, nitrogen dioxide, combustible gases or refrigerants) that themselves may present a risk to maintenance personnel in mechanical rooms. Training is a critical activity to mitigate these risks.
HEPA filters with inadequate seals and breaches in the filter media can cause contaminants into occupied spaces. Regular inspections and maintenance can mitigate those issues.
Water systems
Plumbing systems containing water can be affected by well-known risks, including but not limited to Legionella. Most of the industry resources that informed hospital water management programs in the mid-1990s have been recently updated. The updated ANSI/ASHRAE Standard 188-2018, Legionellosis: Risk Management for Building Water Systems, establishes minimum Legionellosis risk management requirements for building water systems.
A medical air compressor supply system must be maintained in accordance with manufacturer’s recommendations per NFPA 99-2012, 5.1.14.4.7(1), and particular attention should be paid to the common mode failure potential of the control panel power source.
Image courtesy of ASHE
The Centers for Medicare & Medicaid Services’ June 2, 2017, CMS QSO-17-30-Hospitals/CAHs/NHs, document on “Requirement to Reduce Legionella Risk in Healthcare Facility Water Systems to Prevent Cases and Outbreaks of Legionnaires’ Disease (LD),” which was revised on July 6, 2018, mandates “developing and adhering to policies and procedures that inhibit microbial growth in building water systems that reduce the risk of growth and spread of Legionella and other opportunistic pathogens in water.”
The American Society for Health Care Engineering monograph on “Water Management in Health Care Facilities: Complying with ASHRAE Standard 188” is a primary reference.
The CMS document and the related Centers for Disease Control and Prevention’s (CDC’s) toolkit, titled “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings — A Practical Guide to Implementing Industry Standards,” informed most hospital water management programs.
The recently published ASHRAE Guideline 12-2020, “Managing the Risk of Legionellosis Associated with Building Water Systems,” is also now under continuous maintenance; on the training side is ASSE/IAPMO/ANSI 12080, Professional Qualifications Standard for Legionella Water Safety and Management Personnel.
The water management protocols that hospitals established several years ago are not necessarily cast in concrete. For example, the COVID-19 changes impacting some health care facilities created previously unexpected changes to health care facility usage, including water usage. Some of these unexpected impacts may have resulted in low-flow conditions and occupancy changes. Water management plans may need to be updated.
Another major potential risk is the loss of safe water service. The causes can include adverse weather events, pumping station failures, contamination, external or internal pipe breaks, and more. The CDC, the Department of Health & Human Services and the Environmental Protection Agency have also recently updated an excellent resource titled “Emergency Water Supply Planning Guide for Hospitals and Healthcare Facilities,” and have additionally supplemented the guide with a shorter summary.
Gas and vacuum
Piped gas and vacuum systems within health care facilities are covered by NFPA 99, Chapter 5, Gas and Vacuum Systems, and Chapter 11, Gas Equipment. Both chapters have numerous detailed requirements, and those who work with these systems should be conversant with all relevant detailed requirements.
Resources
Chapter 5 is split into three sections by risk category, with 5.1, Category 1 Piped Gas and Vacuum Systems, being the highest risk. Many historical risks have already been addressed by the installation, operation and testing details within NFPA 99-2012. The clearly mandated signage and labeling requirements, many of them retroactive to existing piping systems and locations, are one example. Other examples include restrictions on locations for medical air system intakes as well as for medical vacuum system and waste anesthesia gas discharge (WAGD) exhaust points.
An example of these risks is the danger from cross-connecting different gases. Another example is the statement in 5.1.2, Nature of Hazards of Gas and Vacuum Systems: “Potential fire and explosion hazards associated with positive pressure gas central piping systems and medical-surgical vacuum systems shall be considered in the design, installation, testing, operation and maintenance of these systems. In medical gases, there seems to be general agreement that standards are achieving much of their original goal of mitigating construction-related hazards. As a result, the problems now being reported are more likely to relate to the operation and maintenance of the systems. One of the major additions to the 2012 edition of NFPA 99 is more extensive guidance on maintenance, which is found in 5.1.14.2.”
An article in the September 2016, Volume 19, Issue 9, edition of Joint Commission Resources’ Environment of Care News states: “NFPA 99 defines medical gases used for medical care/treatment as medical air, oxygen, nitrous oxide, carbon dioxide and helium. With the exception of medical air, these can present significant hazards to patients, staff and visitors, including improper venting, violent reactions when gases interact with other incompatible gases or materials, fire safety risks, and displacement of gases in a confined space thereby reducing the amount of breathable air.”
The rapid health care systems’ infrastructure ramp-ups to the early 2020 COVID-19 responses included adding many new piped gas devices in short order. Those devices must be included within the appropriate inventories so that they are rolled into the ongoing inspection, testing and maintenance requirements of the organization to reduce future risks and maintain system safety.
Electrical power
One risk affecting hospital electrical power systems is the increasing likelihood of incoming electric utility outages.
Available resources addressing electrical utility outages that can adversely affect health care facilities include the Department of Health and Human Services’ Sustainable and Climate-Resilient Health Care Facilities Initiative (SCRHCFI) and SCRHCFI Sustainable and Climate-Resilient Health Care Facilities Toolkit.
These resources are useful in addressing Chapter 3 of the Department of Energy’s Quadrennial Technology Review – An Assessment of Energy Technologies and Research Opportunities, and indicated both a trend toward more frequent and intense weather-related electrical power grid disruptions with major disruptions every few years, and the potential for cyberattacks or physical attacks on the electrical power grid.
From an internal perspective, years of deferred maintenance of many power system components such as switchgear, switchboards, motor control centers and panelboards may also cause a higher incidence of future internal equipment failures. Regular thermographic scanning of this equipment can help facilities professionals anticipate future failures before they occur.
The increasing use of new clinical technology on health care power systems before 2020 was discussed in an article titled “Powering Up: The growing electrical requirements for health care technology,” which appeared in the November/December 2019 issue of Health Facilities Management (HFM).
That growth has accelerated even more drastically in 2020 by the impact of the COVID-19 pandemic on rapidly growing telehealth usage, acceptance and capabilities throughout the American health care infrastructure. In the HFM article’s sidebar, the prediction of increasing utilization of the emergency power supply system and its broader extension, the essential electrical system, was identified to be beyond the historical codes and standards requirements to reflect that many health care facilities will be determined to successfully operate in island mode even with a nonfunctioning incoming electrical utility service.
For a more extensive treatment of this issue, including improving both electrical power equipment maintenance and other mitigating approaches, readers can refer to the April 2020 article in HFM titled, “Seven factors to monitor in power system operations.” They may also refer to the March 2019 article titled, “Time for a power system reliability check: Emergency equipment receives much attention, but normal power infrastructure requires scrutiny, too.”
Proactively performing
Effective risk management involves proactively performing risk assessments.
When risks are identified, facilities professionals should consider standardizing risk-mitigating practices when appropriate, and train responders in those practices.
Additionally, they should establish an internal culture where staff are encouraged to report risks.
David L. Stymiest, PE, CHFM, CHSP, FASHE, is a senior consultant at Smith Seckman Reid, Nashville, Tenn. He can be reached at dstymiest@ssr-inc.com.
The following documents were discussed in this article:
- Anesthesia Patient Safety Foundation: "Humidity Levels in ORs."
- "APIC Infection Preventionists Guide to the OR."
- ASHE monograph: “Water Management in Health Care Facilities: Complying with ASHRAE Standard 188.”
- "ASHRAE Position Document on Airborne Infectious Diseases."
- CDC toolkit: “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings — A Practical Guide to Implementing Industry Standards.”
- CMS: “Requirement to Reduce Legionella Risk in Healthcare Facility Water Systems to Prevent Cases and Outbreaks of Legionnaires’ Disease (LD).”
- Department of Energy: Chapter 3 of Quadrennial Technology Review – An Assessment of Energy Technologies and Research Opportunities.
- "Emergency Water Supply Planning Guide for Hospitals and Healthcare Facilities."
- "Emergency Water Supply Planning Guide For Hospitals and Healthcare Facilities Grab-and-Go Summary."
- SCRHCFI: "Sustainable and Climate-Resilient Health Care Facilities Toolkit."




