Emerging technologies impact hospital infrastructure and design
Emerging technologies dramatically will change health care in the near future. They are providing improved patient outcomes and creating new health care delivery methods. New health care facility design requirements and adaptive technology-implementation strategies will be needed to stay in front of these changes.
Programming elements
Patient care methods and processes are being changed by a multitude of developing technologies. These include:
- Augmented reality (AR). This is real-time digital integration of information and images into the user’s environment. AR technologies like mixed-reality smart glasses are providing technical support and decision support, both in the clinical environment and the facility design process.
- Virtual reality (VR). This is an interactive computer-generated 3D environment. VR technologies are transforming health care in predictive clinical simulations, neurorehabilitation, pain management, education and more.
- Artificial intelligence (AI). This means computer systems that are programmed for simulated human thinking, including machine learning. AI solutions are providing predictive analytics with better clinical outcomes.
- 3D printing. This is an additive printing process creating three-dimensional solid objects from a digital file. Health care utilization includes customized implants, custom prostheses, bioprinting for burn victims and much more.
Universities and teaching facilities have been leading the charge by adopting technology tools to teach students and residents. For instance, the Ichan School of Medicine at Mount Sinai in New York City is utilizing AI to evaluate medical records to predict patient disease risks, and the University of Rochester (N.Y.) Medical Center is 3D printing lifelike artificial organs and human anatomy for realistic surgical simulations. Companies have even developed platforms that allow surgeons to practice surgical techniques in a virtual environment, which can reduce risks to patients. These educational techniques have laid the groundwork for clinicians to embrace technologies in many other areas.
Sutter Health utilizes AR via Google Glass smart glasses, which integrate a patient’s medical records and streams the visit to a scribe located in a remote facility. This allows the clinicians more direct patient interaction during clinical assessments, provides instant documentation and reduces the need for documentation stations in the clinics because information is displayed on the glasses. Likewise, Duke University in Durham, N.C., is exploring augmented reality by transposing a computed tomography (CT) image onto the patient, assisting neurosurgeons during emergency procedures.
Some facilities are even trialing Microsoft’s HoloLens to project a CT model rendering of the spine onto patients to aid surgeons in screw trajectory placement. One company has even developed a mobile AR solution to assist paramedics with augmented decision support and ability for remote consult with an emergency department (ED) physician.
Each of these technologies requires new considerations for workflow, space adjacencies, clear floor area requirements and infrastructure. Adjustments to existing master plans, space programs, building designs, infrastructure and systems integrations will be needed to address these technologies.
Technology master planning
The convergence of AR, VR, AI and 3D printers with medical devices, building systems, electronic health records and infrastructure require new design considerations. These items create workflow challenges, systems integration issues and a need for changes in our health care design solutions to meet the demand of these new technologies.
Facilities must develop clear action plans to address these complex technologies, and it begins with engaging the clinical leadership team to capture their vision for the next 10 years. Just as facility professionals have developed facilities master plans, it is critical that a health care technology master plan be developed that aligns with the health system’s clinical and operational goals. Participants in developing this technology vision should include key staff from biomedical, information technology (IT), facilities, supply chain, administration and other hospital departments. This comprehensive team approach helps ensure that needs and expectations are captured.
Technology visioning session topics should go well beyond systems and devices currently used in a facility. Discussions about industry technology trends such as AR, VR, AI and 3D printing must be addressed and timelines assigned for potential roll-outs. This will help the team evaluate short-term plans to address infrastructure, systems integrations, space needs and resiliency requirements. Key planning considerations include the following:
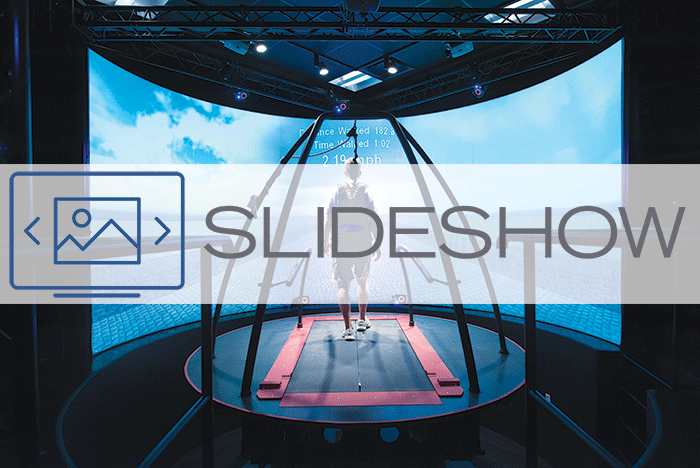
• Functional challenges. As VR and AR continue to expand into clinical training and continuing education, facility training areas and simulation rooms will need to support fixed equipment and mobile AR and VR equipment. Dedicated VR staff-training spaces also should be considered to practice surgical procedures and clinical simulations. Whether fixed or portable, VR systems require clear floor areas, specific sensor placement and robust infrastructure.
VR utilized for physical rehabilitation may require exercise equipment and large monitors for physical therapists to interact and direct patient movements. VR also has found clinical application in mental health treatments, neuro/stroke rehabilitation, surgical-procedure training and virtual telepresence in remote facilities that provide team collaboration and consultation.
AR clinical team-support locations and touchdown areas are needed to address remote AR consults. These consult spaces may be for dedicated AR clinician support in an off-site office building, a specialist providing remote diagnosis to patients in a regional clinic, or an ED physician providing urgent consults.
These AR spaces can be combined with virtual care touchdown areas within hospital units for clinician interactions with remote patients and general team collaboration. The actual AR devices, such as the HoloLens, are portable, and technology considerations primarily focus on the need for charging stations, wireless infrastructure, system interfaces and infection control protocols.
AI and data analytics are increasing patient safety and providing better clinical outcomes. These solutions utilize massive amounts of data and, when combined with the growth in biometric patient monitoring, most facilities’ data centers are inadequate to meet demands. On-site data center growth combined with cloud-based data solutions should be evaluated as part of an overall strategic plan.
AI is data-driven, but real-time visualization and notification to clinicians should be planned. For instance, Indiana University Health in Indianapolis created a data visualization platform using predictive analytics, which provided visual alerts to clinicians to aid in fighting infections. These AI alerts can be in the form of wall monitors, personal computers and integration to wireless phones, but should be customized to meet clinical requirements.
• Physical space. AR, VR, AI and 3D printing present an array of space-planning options to consider and align with an overall technology vision. Virtual care and AI monitoring of high-risk inpatients and outpatients via biomonitoring sensors continue to grow. These developments will push the need for remote dashboard monitoring within the facility and remote command centers as well as mobile solutions.
Clinical command centers and virtual operations centers will be needed at various levels as facilities adopt these technologies. For instance, NewYork-Presbyterian in New York City recently developed a version it named the Clinical Operations Center. This space infuses AI with patient monitoring and nurses to remotely monitor patients on hospital units, helping to reduce adverse events. Each facility’s requirements should be tailored to the overall technology vision and should be included within facility master-planning activities.
3D printing is well-positioned to be a positive disruption in the health care industry, providing numerous options. Cleveland Clinic has developed an innovative 3D printing technique to manufacture custom airway stents for patients to help with breathing. Other 3D printing developments are rapidly progressing that provide custom surgical instruments, casts, bone implants, prostheses, pharmaceuticals and even printed supplies on demand.
These printing applications create new workflows and space requirements that range from a basic countertop area to clean core work area to dedicated clean rooms for bioprinting. Each clinical process and workflow should be analyzed to determine proper adjacencies and access.
As each of these diverse technologies floods the health care industry, additional IT and biomedical staff will be required. To meet these different demands, some will be needed at the hospital, others at regional clinics, and some will be mobile. These IT/biomedical teams will need additional support spaces with staging and workbench areas. Some of these team members will be addressing the AI needs of data mining and analytics. These AI teams need open office space and conference rooms to support the development of project analytics. Charting these staff additions in conjunction with the technology vision timeline should be incorporated into the facilities master plan.
• Technology integration. AI, AR and VR can go far beyond image visualization and data mining of electronic health records for clinical reports. Integrated home monitoring of high-risk patients’ biosensors and miscellaneous data sets to support virtual care centers is a prominent example that is growing rapidly.
AI decision support solutions continue to advance in many areas such as the IBM Watson project. This project has provided precision medicine immunotherapy-treatment recommendations based upon analyzing patient-specific records, industry standards and clinical trials.
AI provides endless possibilities such as addiction treatment via a predictive patient-monitoring app that notifies the clinical team to engage when relapse risks are high. Another example is integrating AR headsets with nurse call, real-time locating systems and patient data to help improve staff efficiencies.
All of these technology integrations span across medical equipment, IT equipment, communications equipment, building systems and even the “internet of things.” In addition, all of these solutions must be monitored by clinical and technical teams. A multitude of team members representing various systems, platforms, departments and companies are required to address the complex integrations needed for these solutions.
The challenge is to define clearly the clinical goals with technical requirements. An effective way to address this issue is by developing a detailed workflow diagram that defines the clinical operational needs and expectations. This serves as a quick method to produce a document for all technical team members to determine integration requirements, systems issues and assign clear responsibilities for resolution.
As with most complex technologies, ongoing support is the key to successful implementation. The convergence of these technologies is further complicated by the number of diverse technical team members needed to troubleshoot a single integration issue. Facilities will need to implement detailed trouble-ticket protocols for vendors and staff across different departments. In addition, facilities must be prepared to provide tech support of remote home-monitoring devices.
• System resilience. As AI, AR, VR, 3D printing and similar solutions are intertwined into care delivery, dependence on technology in the clinical environment is being substantially increased. Interdependencies and connectivity have become critical for patient care. Traditionally, this was limited to the hospital but today interdependencies between facilities are critical to care delivery. A symbiotic health care ecosystem is growing in health care with technology as the key vessel for clinicians. Remote AR consultations, e-visits, telemedicine, e-pharmacy, AI clinician decision support, AR consults, remote monitoring and clinical team video collaboration are all interconnected.
Health facility professionals plan for power outages and other challenges, but the disaster recovery plan must be broadened to avoid disrupting care.
Considerations for remote clinics, remote patient monitoring, telemedicine connectivity, database connections and the home hospital are a must. This begins with a robust wide area network infrastructure not just within the four walls of the hospital. Resiliency of the service providers must be evaluated thoroughly, ensuring that network connectivity from the service provider is routing two different directions out of each site as well as routing them to two different telephone company providers.
Cellular data connectivity also can be considered as an added element of the overall disaster-recovery plan.
Ensuring that redundant power is provided on key mission-critical equipment and connections that impact patient care should be implemented. Emergency power may even be needed in areas such as clinics and virtual care centers.
Ultimately the resiliency of AI, AR, VR and other technologies must be evaluated as part of a large ecosystem that is completely interdependent. Involving key clinicians and stakeholders from IT, biomedical and facilities departments to evaluate from a holistic perspective will help ensure that all services remain active to support mission-critical care delivery.
A key component
AR, VR and AI in health care are expected to grow 35-40 percent by 2023 and 3D printing in health care is also expected to grow quickly. To support this growth, health care technology must be a key component of a health facility professional’s strategic facilities master plan.
Ted Hood is associate and senior project manager at TLC Engineering for Architecture, headquartered in Orlando, Fla. He can be reached at ted.hood@tlc-eng.com.