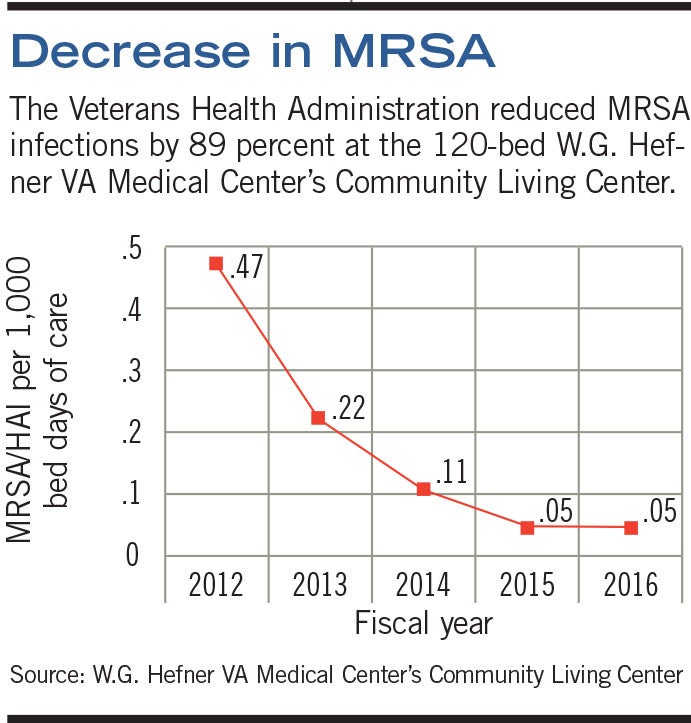
VHA initiative reduces MRSA 89 percent in veterans’ center
An initiative led by the Veterans Health Administration (VHA) reduced methicillin-resistant Staphylococcus aureus (MRSA) infections by 89 percent over four years at the 120-bed W.G. Hefner VA Medical Center’s Community Living Center (CLC) in Salisbury, N.C.
Active surveillance and decolonization combined with a strict environmental services (ES) regimen contributed to the reduction, according to the study’s lead author, Lanette Hughes, R.N., infection preventionist at the CLC. At an estimated cost of $28,000 to treat each MRSA infection, researchers projected that the initiative saved roughly $2.2 million by preventing an otherwise expected 64 infections over the study period of 2013-2016.
Results of the research were presented at the Association for Professionals in Infection Control and Epidemiology’s (APIC’s) 44th annual conference in June. “This research shows the positive impact that targeted infection-prevention interventions can have on patient safety and health care costs,” says Linda Greene, R.N., president of APIC.
The aggressive intervention was put into place after a previous attempt to stop the spread of MRSA in 2007 proved unsuccessful. That effort relied on contact precautions — isolating colonized residents, using dedicated medical equipment for each resident and requiring health care workers to don gowns before entering rooms.
Despite implementing the strategies, the prevalence of MRSA colonization climbed to 70 percent of residents and 19 MRSA infections by 2012.
Hughes explains that each year an estimated 30 percent of the CLC’s admissions are already colonized with MRSA; the center is a long-term residence for many and a permanent home for others.
As more residents were admitted already MRSA-colonized, the environmental burden increased and more residents became colonized, which put residents at a higher risk of infection, Hughes says.
The increased colonization rate led researchers to consider taking actions over and above contact precautions. Beginning in 2012, the CLC staff began testing all MRSA-negative residents and then decolonizing all known positives, plus everyone who tested positive at that time for five consecutive days. Decolonization consisted of daily chlorhexidine bathing and the use of intranasal mupirocin ointment.
In addition to the decolonization, ES staff performed daily terminal cleaning of each resident room, bathroom and all common areas, including utilization of ultraviolet C (UVC) light for added control of the environment. Wheelchairs, walkers and scooters also were cleaned daily and treated with UVC light.
The MRSA colonization prevalence rate decreased from 45 percent of residents in the first quarter of 2013 to 16 percent in the fourth quarter of 2013. The number of MRSA infections dropped from 19 in 2012 to two in 2015 and 2016.
“The cornerstone was strict environmental control, decontamination and cleaning,” says Hughes.