Money well spent
 While health facility teams work diligently to meet their dynamic and extensive capital needs, a growing demand for state-of-the-art infrastructure, increasing safety regulations and an influx of patients add extra strain to daily operations. Health care organizations are challenged with various resource-intensive projects, making capital increasingly scarce for hospital facility managers. Without a strategic plan to ensure that capital spending is aligned with capital plans and budgets, health facility managers run the risk of misallocating precious capital in less than optimal ways.
While health facility teams work diligently to meet their dynamic and extensive capital needs, a growing demand for state-of-the-art infrastructure, increasing safety regulations and an influx of patients add extra strain to daily operations. Health care organizations are challenged with various resource-intensive projects, making capital increasingly scarce for hospital facility managers. Without a strategic plan to ensure that capital spending is aligned with capital plans and budgets, health facility managers run the risk of misallocating precious capital in less than optimal ways.
An efficient capital spend management system provides a real-time, reconciled view of overall capital spending, helping hospital facility managers control ongoing capital spending against the planned budget. Deploying a capital spend management system provides standardized, automated solutions for three key areas of vulnerability within hospital facilities management — accountability, communication and process efficiency.
To address these areas of vulnerability within hospital facility management, capital spend management incorporates best practices that help facility managers mitigate risk and lower cost while maintaining high levels of quality and efficiency.
Validation and accountability
An accountable capital spend management process enables hospital facility managers to validate budgetary needs, receive adequate funding and meet all necessary capital needs within the budgetary requirements. Hospital facilities managers can work to achieve excellence in two key areas of accountability — data centralization and accuracy of information.
Typically, capital spend data is distributed across many departments and silo'd among various roles, as opposed to being centralized, highly visible and immediately accessible to key stakeholders. For example, data is often contained in spread sheets, emails, handwritten notes and other disparate sources that drive segments of the capital spend process throughout a health care organization. Rapid reconciliation of spending is exceedingly difficult due to the manually intensive data collection process. Long lag-times result, making capital misallocation more likely. Poor visibility into the data and an ill-defined workflow slows down the decision-making process and weakens the ability to control spending. Without visibility into and control of all strategies, processes and systems, financial and facilities departments are unable to fully optimize capital spending.
 |
| UMass Memorial implemented capital spend management software that provides greater visibility into and efficient control of all expenditures. |
A successful capital spend management system replaces typical disparate data sources with a central repository for data. This adds a level of accuracy, convenience and structure for all stakeholders who need access to the data. Once data is input into a centralized system, it is available for data management, tracking and reporting. A real-time approach allows immediate access to spending data, eliminating the lag-time between requisitions, approvals and reconciliations. In addition, a centralized repository of data provides the visibility and transparency the financial team needs to minimize unplanned expenditures and budget overruns.
Essentially, health facility managers improve accountability through centralizing and maintaining validated and accurate information. When facility managers can demonstrate accountability for budgetary decisions, other stakeholders are willing to take a more proactive role in the capital budgeting process.
Improving communication
Health facility managers with a strong capital spend management system are well positioned to improve communication. Effective communication has an extremely significant impact on the overall success of a capital spend plan; the key is to promote engagement, alignment, integration and collaboration when communicating.
You may also like |
| The case for infrastructure spending |
| Outpatient MEP and technology infrastructure |
| |
The capital budgeting process is often an annual, static financial event. A capital spend management system creates a dynamic, ongoing fiduciary management process, accommodating any unforeseen needs and strategic opportunities that may emerge throughout the year. For example, when requisitions are made, departmental managers must obtain approval before taking action. With a centralized capital spend management system in place, stakeholders can readily engage in the requisition process because information is visible and available for all to see and use. Another example, budget overages, often occurs without awareness or approval from key support areas within the organization. A capital spend management system provides a convenient, structured environment for stakeholders to engage in the daily process of approving and tracking spend. It also provides a workflow for communication that lets everyone know where projects stand at all times. Having structured communications helps increase the engagement of stakeholders with the capital budgeting process.
Ensuring that spending plans are aligned with the business objectives of an organization is another important best practice that results from good communication. Often, the capital spend approval process is not strictly monitored, creating distance between finance departments, project management and contractors. A capital spend management system closes this gap through a disciplined and real-time approach, enabling departments to set project budgets that are aligned with the organization's strategic objectives. This ensures that all spending plans are communicated throughout the organization, providing all appropriate stakeholders with the real-time information necessary to prioritize spending plans that directly support long-term strategic goals.
Within a health care organization, there are usually many departments involved with the capital budgeting process, including finance, facilities, engineering, IT and others, as well as the medical departments. Without a means to integrate these key areas, capital budgets may not be accurate and result in unwanted surprises to facility managers or to the finance department. A capital spend management system helps integrate organizational communication through a comprehensive review and approval process. Multiple departments are provided the real-time information that helps an organization integrate its capital budgeting process. Capital spend management increases the quality of collaboration at an organization through a high level of enterprisewide visibility. Additionally, real-time reports can significantly increase data visibility and collaborative decision support. With a platform to actively communicate throughout the planning and purchasing process, organizations can collaborate to form more accurate, realistic and comprehensive capital budgeting plans.
Standardization increases efficiency
Without standardization, the capital budgeting process is frequently riddled with inefficient, manually intensive processes. Data is manually collected and consolidated into a master spreadsheet to determine total capital spend for projects, but this process often lacks consistency and data integrity. After weeks or months of data aggregation, the master spreadsheet is used to create budget tracking spreadsheets and software systems for each project, again decentralizing the data. This prevents the ability to drill down on line item details, especially in real-time, rendering any analysis of planned and actual spending out-of-date. Also, regional facilities and even individual departments are often used to using their own processes for budgeting and requisition, with no roll-up to a central budgeting and approval process. In the end, this capital budgeting approach can lead to overspending on materials, equipment and resources.
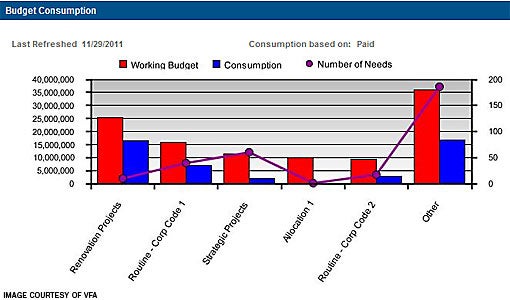 |
| Capital budget allocation dashboard highlighting budget consumption per capital program. |
A capital spend management system can improve standardization, eliminating inefficiencies and increasing simplicity, structure and consistency through automation. The first major benefit of automation is the elimination of the potentially error-prone paper-driven process. Automating data aggregation into a central repository eliminates the need for project managers to individually manage purchase orders, invoices and total spending for each project with separate spreadsheets. Automating the requisition and approval process adds visibility, authority and accountability to the capital budgeting process. This significantly reduces processing time while providing better information to the departments involved. Process standardization structures capital spend data for dynamic and consistent reporting.
With process standardization, health facility managers increase the efficiency of daily operations, creating more time to focus on life-safety issues and other critical needs. More focus can be placed on project responsibilities by reducing the time spent on manual processes, as well as the time it takes to identify a need, receive approval and make a purchase. Reducing the cycle time to generate and reconcile capital spend reports enables managers to easily track variances of all planned, budgeted, forecasted and actual capital expenditures. The processing time it takes to go from requisition to a purchase order can be reduced to a fraction of the time with process standardization. Through process standardization, health care facility managers have tighter controls over the capital budgeting process.
Successes the field
Catholic Health Partners (CHP) is the largest health system in Ohio, with more than 4,800 acute beds spanning many hospitals, service and wellness centers. CHP has been named a top health system in the United States for quality and efficiency by Thomson Reuters three years in a row.
CHP had struggled with the costly challenges that contribute to effectively allocating capital, including accurate information on expenditures, quick reconciliation of spending, visibility and transparency into the budget planning process and surprise expenditures. CHP wanted to demonstrate greater returns on capital investments and provide greater visibility of spending across the organization.
In a health care organization, technology, regulations and procedures are always changing. For this reason, CHP needed a mechanism to more efficiently plan future spend, especially in regards to large capital projects. CHP needed a common platform for its regions to track capital spending against their budgets. The solution had to provide an enhanced ability to identify system group capital purchasing opportunities, as well as enhanced reporting and tracking tools to manage construction projects.
CHP selected capital spend management software that would help to consolidate finance and project data. It provides an end-to-end solution that centralizes capital planning and expenditure tracking, automating review and approval processes and accurately monitoring all capital projects. The solution provides tighter control and, therefore, optimized use of capital.
CHP now has a more consistent means of tracking and reporting on large construction projects, standardization of data input/output, the ability to identify group purchasing opportunities across the system and a collaborative environment for executives to strategically manage capital budgets. There is transparency in the administration of the capital budget for both the regions and the system. Regional executives now have the ability to process approvals electronically. CHP can now look at all capital needs holistically and think more strategically about what projects should move forward.
Likewise, UMass Memorial Health Care is the largest health care system in Central and Western Massachusetts, and clinical partner of the University of Massachusetts Medical School. The system includes UMass Memorial Medical Center, four community hospitals, home health and hospice programs, behavioral health programs and physician practices.
The capital planning and management group faced several challenges. Existing processes to track budgets and spend were manually intensive, using a master spreadsheet to determine the total capital spend per project. Active project budgets were tracked in a different spreadsheet, and purchase orders were issued and tracked in a separate system. The same data was entered into multiple systems. The capital spend approval process was not strictly monitored, and the project manager and contractors lacked clear communication channels for approved spend.
UMass Memorial developed a capital spend workflow — documenting the most effective course for managing, approving and tracking projects into a crucial central repository. Based on this workflow, they wanted to input and manipulate data within one system for data management, tracking and reporting.
UMass Memorial implemented capital spend management software as the budget, approval and requisition answer they required. The web-based solution provided a convenient, structured environment for all stakeholders to document, forecast and track activities related to capital expenditures.
UMass Memorial now refers to the spend management system as its "internal clearing house," because they use it to automatically aggregate data from both the purchase order system and accounts payable system, eliminating the need for separate tracking. A direct connection between the spend management system and the general ledger enables the finance group to run reports and diagnose progress. The ability to run real-time reports also significantly increases UMass Memorial's informed decision support.
UMass Memorial has redefined the capital management processes and now has an automated and centralized solution that provides greater visibility into and efficient control of all planned, budgeted and actual capital expenditures.
Centralized management benefits
A solid capital spend management system brings a number of benefits to a health care organization. To increase accountability, information is centralized for more visibility, structure and accuracy of data. Communications are improved through a system that supports proactive engagement, integration and alignment among stakeholders for effective collaboration. Process standardization and automation frees up resources for optimal use, resulting in efficient operations that provide facility managers with more control, focus and agility when planning for capital spend needs. Implementing these best practices through a structured capital spend management system helps health care organizations to meet the goal of mitigating risk and minimizing cost.
Keith O'Leary is director of product marketing for VFA Inc., a Boston-based provider of software and services for facilities asset management and capital planning. He can be reached at koleary@vfa.com.




