Infrastructures to improve patient safety
 |
| Photo by DragonImages |
Patient falls were the largest category of adverse events reported several years ago at Barnes-Jewish Hospital, St. Louis.
While the hospital had purchased a portable bed exit alarm system, problems persisted because the unit often was unavailable, resulting in delayed care delivery and staff dissatisfaction.
To help alleviate these difficulties, hospital staff mounted the portable bed exit alarm devices from Stanley Healthcare, Waltham, Mass., above each bed in two intervention units.
You may also like |
| Upgrading nurse call systems |
| Managing clinical alarms for safety |
| Reducing workplace violence incidents |
| Emergency power for patient safety |
| |
In the first six months of 2009, the fall rate in one intervention unit decreased from 4.48 to 1.96. While the second unit saw only a slight decrease in its fall rate during the period, its injury rate decreased from 1.56 to 0.
Right device, right application
As hospitals continue to improve their patient safety practices, technology and engineering infrastructures are becoming the backbone of many of these efforts.
Whether it’s supporting high-tech devices that help to ensure the physical safety of patients, HVAC systems that maintain the optimal airflow to help prevent infections, power management equipment that helps to establish a safe environment under extraordinary circumstances or plumbing systems that provide high-quality water for disinfection efforts and safe patient use, this infrastructure delivers essential support for human interventions.
But, as demonstrated by Barnes-Jewish Hospital, many of these devices and systems can only reach peak performance when planned, installed and managed collaboratively between designers and operators.
“I think there’s a challenge in that many engineering solutions or activities happen in comparative isolation,” says Michael Bell, M.D., deputy director of the Centers for Disease Control and Prevention’s division of healthcare quality promotion. “If [collaboration] would become more the norm rather than the exception, there might be some unexpected benefits that could be realized.”
Health facilities professionals must keep these challenges in mind as they explore the wide variety of technology and engineering solutions coming to bear on the patient safety issue.
Additional resource |
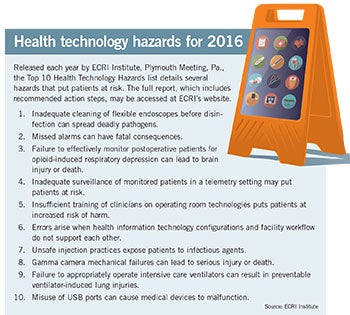 |
| This graphic shows the top 10 health technology hazards for 2016. |
Technology solutions
“A lot of institutions are focusing on technical safety features because of changes to reimbursement policy,” says Debbie Gregory, R.N., senior clinical consultant for clinical innovation and transformation at Smith Seckman Reid Inc., Nashville, Tenn. “From a technology standpoint, much of it has to do with patient tracking, patient falls, infection prevention — those types of things.”
Some of the simplest patient safety solutions can be accessed through the latest generation of nurse call systems, Gregory says. “There are many safety features available within the modern nurse call workflow station, such as rounding or reminders. If you give someone pain medicine, for example, you can set a reminder to come back and check for pain relief within so many minutes. You also can set a reminder for rounding, safety checks, or anything.”
Other technical functions can be housed on the facility’s wireless information infrastructure or as stand-alone systems that sometimes interact with other information systems, depending on the performance and capacity needs.
“The advantage to using the Wi-Fi system is there’s potential cost savings because you’re going to be utilizing the existing network,” explains Tod Moore, principal and discipline lead for information and communication technology at design firm Stantec, Lynnwood, Wash. “The disadvantage is that you’re using a system that supports many different applications, such as voice, data, video, security, wireless clocks and some telemetry systems, so it can become burdened if you try to add something like a real-time locating system (RTLS) on top of that.”
However they’re configured, the key goal of these technologies is to provide additional patient safety efficiently.
“For instance, patient tracking through RTLSs can help an organization establish a second pair of eyes or second source of data to ensure that there’s enough time to respond to a situation,” says Gregory. “And you might even have some analytics ahead of time to predict some of those situations, like patient falls.” Tracking Alzheimer’s patients to prevent wandering is another possible use for RTLS, she adds.
Additional resource |
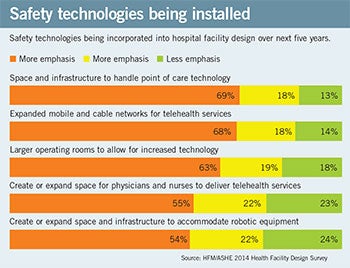 |
| This downloadable chart Shows which safety technologies are most likely to be installed in hospital facilities. |
Gregory allows that some hospital “smart beds” also have useful patient movement- and fall-detection features.
The staff-locating functions of RTLSs also can add to an organization’s patient safety efforts, Gregory says. “For staff locating, they can see how often the staff go into the room, just to be able to identify if there were a fall and how often the nurses had come into the room,” she explains. “So it can provide a precautionary measure to improve observation, as well as an accountability measure.”
RTLS technologies such as radio-frequency identification (RFID), infrared (IR) and ultrasound-based equipment also play key roles in hand-hygiene monitoring systems, Moore says.
“Obviously, the hand-hygiene issue as it relates to technology is a pretty big deal because it affects infection control as well as HCAHPS scores,” says Moore. “By utilizing RFID technology potential coupled with IR or ultrasound technology, the hand-hygiene dispensers can track usage, so it knows that a nurse, doctor or clinician came into the room and whether or not he or she used the hand-hygiene dispenser.”
Moving closer to the clinical area, health care institutions and vendors are continuing to develop new ways to bring the benefits of medical equipment alarms to institutions without the problems of alarm fatigue, which has become a Joint Commission National Patient Safety Goal, says Rikin Shah, senior associate in the applied solution group at ECRI Institute, Plymouth Meeting, Pa.
“It’s an organizational, cultural and technology issue,” says Shah. “It’s looking at how you are going to change your practices to mitigate alarm fatigue and change the way you utilize and implement the technologies that are in your facilities.”
The fatigue issue has become particularly acute due to the proliferation of clinical alarms and the growth of personal communication devices for clinical staff.
One key to preventing alarm fatigue is to change alarm limits to the patient demographic so clinical staff will receive an alarm only if the condition is actionable for the specific patient and not a “one-size-fits-all” alarm for healthy and unhealthy patients alike, Shah says. Another protection involves implementing middleware that collects alarm data from medical devices and prioritizes the alarm type and recipient of the alarm, thus avoiding all alarms going to all caregivers all the time.
Security and life safety
Perhaps because they’ve been long-held concerns for health care facilities, many physical security and life safety devices tend to use more mature patient safety technologies. However, some of these systems are expanding their features as they connect to wireless and IP-enabled infrastructures.
Infant abduction-prevention systems traditionally have sounded alarms when infants are moved through a doorway or near another exit point, but additional capabilities can be used to track infant movement throughout a facility as well as connect to communication platforms throughout a facility or campus.
“When there’s a problem, visual and audio alarms will go off, as well as indicators associated with the nurse call system and their monitors,” says Moore. “Then, the door or elevator or whatever access point is being breached will be locked down for as long as codes allow.” Video surveillance also can be tied into the system, he adds.
Another mature technology getting an upgrade through integration with other security devices is a variety of access control devices, including combination locks and card readers. Additionally, Gregory mentions biometric devices and video entry systems as new variations on the access control theme.
A less-common patient safety measure is lobby and visitor management systems, according to Thomas A. Smith, CHPA, CPP, president of Healthcare Security Consultants Inc., Chapel Hill, N.C. These allow staff to run checks on visitors against organization or public databases.
“I tend to look at them in my practice when I’m doing assessments and looking at what people can do to tune up their physical security and operational security measures,” Smith says. “I think they are now becoming more mature and more fully integrated with their current security management systems.”
While fire alarms are required to be on their own systems by code, they also are interfacing with newer equipment to improve patient safety, such as mass notification systems.
“I would say the Virginia Tech shootings spurred more interest in mass notification systems,” says Geoffrey King, principal at Smith Seckman Reid in Dallas. “But they can be used for situations like inclement weather, too.”
Touting their flexibility, King says mass notification systems can be configured to make announcements via mass text messages, overhead speakers or digital signage.
Another emergency response technology that’s getting attention for new construction projects is distributed antenna systems (DASs), which allow first responders to communicate within a building during an emergency, Moore says.
Driven by the communication problems that plagued first responders on 9/11, and the RF-resistant materials used in new construction, DAS also can be used by hospital security and other departments using radios, Moore adds. Another huge component to a DAS is incorporating cellular systems. “Cellphones are a critical part of the communication systems within our health care facilities,” he says. “In order to have coverage inside the building, running them over the DAS becomes a requirement.”
The engineering side
Drilling further down into the patient safety aspects of hospital infrastructure, the world of mechanical-electrical-plumbing (MEP) engineering provides a number of examples of patient safety initiatives.
Much like ECRI Institute’s Shah advocates for clinical alarm limits that fit physiological parameters of each patient, Richard D. Hermans, PE, director of training and advanced applications for Daikin Applied, Minneapolis, speaks of air-quality requirements tailored to the infection control needs of particular patients.
“There’s a public review going on right now on the concept of scaled risk, where you decide which patients to send off to spaces that protect the rest of the occupants in the building and which patients to allow in lower-grade spaces,” says Hermans, who is a member and inaugural chair of ANSI/ASHRAE/ASHE 170, Ventilation of Health Care Facilities, as well as a member of the Facility Guidelines Institute’s steering committee.
Closely related is the growth of off-site health care clinics and other facilities, which are requiring upgraded air circulation to meet the needs of the increasingly acute procedures being performed on-site.
“My personal philosophy is that what’s important in terms of ventilation and controls of air quality in health care has more to do with the procedures that go on in a space than the type of building itself,” he says. “So, for example, a surgery procedure should be treated the same way with regard to ventilation, whether it is in a doctor’s office or an acute care hospital.”
Though mature technologies, such as switches that can quickly bring operating rooms (ORs) up to the required air-change rate, continue to hold hospitals in good stead, newer variations that tie an OR’s HVAC system to its surgery schedule are being introduced.
Hospital engineering departments also are experimenting with ultraviolet light systems placed inside air handlers to keep the growth of bacteria down inside the HVAC systems, as well as different types of air filters.
Beyond these patient safety issues are the age-old questions of optimal humidity levels and air-change rates.
“There was an air-change reduction not too long ago when patient rooms went from six air changes per hour to four air changes,” Hermans says. “And after a long period of debate and research on it, the conclusion was that it’s not going to affect patient safety to go to four air changes.”
Also ensuring patient safety are hospital emergency power systems, which are carrying a lot of the load for the rapid proliferation of patient safety technologies.
“I was just talking to a facility director responsible for a very large hospital, a moderately large hospital and a very small stand-alone emergency department and I asked her about her requests for emergency power,” says David Stymiest, PE, CHFM, CHSP, FASHE, senior consultant for Smith Seckman Reid in Nashville, Tenn. “And she said it’s all about technology because those systems are so power hungry and growing so rapidly — and what she told me doesn’t vary from what I see elsewhere.”
Beyond putting these new technologies on emergency power are the additional requirements needed to power air-conditioning systems to keep data rooms cool during a power problem.
“Another piece is that facilities want more of their HVAC equipment on backup generators because they understand that their technology would fail if the temperatures and the airflows weren’t what they needed to be,” says Stymiest, who is chair of the National Fire Protection Association’s technical committee on emergency power supplies.
Stymiest, who emphasizes that he’s giving his own opinions and not speaking for the NFPA, adds that domestic water also is going on backup power more often than it used to, because it is needed for cleaning and infection control during emergencies.
Indeed, plumbing systems represent another area where engineering professionals are making patient safety strides.
Among the most notable developments has been the publication of ANSI/ASHRAE Standard 188, Legionellosis: Risk Management for Building Water Systems.
“I think that’s a great step forward,” says the CDC’s Bell, “But I’m not sure it’s going to be the final thing.” Citing a need for technical innovation, Bell believes biofilm problems that lead to Legionella ultimately can be solved through design and materials research.
Likewise, Bell cites the need to rethink the design of common plumbing fixtures like hospital sinks and toilets to reduce or eliminate splash plumes.
Innovations ahead
As health facilities professionals continue to play an increasingly larger role in the patient safety equation, Bell believes all parties need to become involved in the facility planning process.
“The question is: How do you get the kind of engineering expertise and infection control know-how involved at the right time when you’re planning a new unit?” he says. “It’s great to focus on an idea — whether it’s water systems or air systems or surface engineering or pathways on the planning process — by having the right people at the table to help drive those patient safety innovations.”
Mike Hrickiewicz is editor of Health Facilities Management.
For more information
The following resources were consulted for this article and offer valuable information regarding technology, security and mechanical-electrical-plumbing infrastructures for patient safety.
• ANSI/ASHRAE Standard 188, Legionellosis: Risk Management for Building Water Systems: https://ashrae.iwrapper.com/ViewOnline/Standard_188-2015
• ANSI/ASHRAE/ASHE Standard 170, Ventilation of Health Care Facilities: https://www.ashrae.org/standards-research--technology/.
• ASHRAE’s Design Manual for Hospitals and Clinics: https://www.ashrae.org/resources--publications/bookstore/hvac-design-manual-for-hospitals-and-clinics
• ECRI Institute’s 2016 Top 10 Health Technology Hazards: https://www.ecri.org/Pages/2016-Hazards.aspx
• Health Facilities Management/American Society for Healthcare Engineering’s 2014 Health Facility Design Survey: http://www.hfmmagazine.com/display/HFM-news-article.dhtml?dcrPath=/templatedata/HF_Common/NewsArticle/data/HFM/Magazine/2014/Oct/cover-health-facility-design-survey
• Health Facilities Management/American Society for Healthcare Engineering’s 2015 Hospital Construction Survey: http://www.hfmmagazine.com/display/HFM-news-article.dhtml?dcrPath=/templatedata/HF_Common/NewsArticle/data/HFM/Magazine/2015/Feb/hfm-hospital-construction-survey
• International Association for Healthcare Security & Safety’s Security Design Guidelines for Healthcare Facilities: https://iahss.site-ym.com/store/ViewProduct.aspx?id=4422798
• Stanley Healthcare’s case studies (listed under “Customers”): http://www.stanleyhealthcare.com/
West Health Medical Technology website: http://www.westhealth.org/
