On alert!
 Medical device alarms alert caregivers to unsafe conditions or changes in a patient's condition that require a response, but the caregiver needs to be within range to hear the alarm.
Medical device alarms alert caregivers to unsafe conditions or changes in a patient's condition that require a response, but the caregiver needs to be within range to hear the alarm.
Some medical devices, such as physiologic monitors, can be networked so that alarm notification not only emanates from the bedside device, but also triggers alarm notification from central stations typically located at the nurses' station. Other enhancements include enunciators that provide audible alarms in locations where it may be difficult to hear device alarms and remote displays in strategic locations that mirror the central station display.
More recently, health care facilities have been considering alarm integration systems as a way of enhancing alarm notification for a wide variety of clinical devices or systems such as physiologic monitors, ventilators, infusion devices, bed exit alarms and nurse calls.
Today's clinical alarm integration systems are highly automated and facilitate the propagation of alarms to a clinician's wireless device, remote displays or even enunciators. If implemented correctly, alarm integration systems can lead to better response times and coverage. However, if incorrectly designed, they can add multiple failure points and place a patient in jeopardy.
Integration system design
Alarm integration systems are complex and require a multidisciplinary approach to planning, design and implementation. Each hospital's system must be customized to the specific area's workflow to effectively enhance alarm notification and facilitate prompt alarm response. Because of this, hospitals must take a deep look at their care areas and alarm management practices as well as their culture, infrastructure and technology.
Each system is designed for a specific facility. However, all clinical alarm integration systems take all or a subset of alarms from a monitoring system and communicate them to a desired location and all have software and hardware components. In general, alarm integration systems share the following building blocks:
Alarm source. This includes nurse call systems, physiologic monitors, ventilators, infusion pumps and many other clinical devices.
Middleware. These are systems or engines that reside between the medical device and a communication device worn by clinicians. The tasks of these systems are to collect all alarms from the source device and to distribute them to the communication devices.
Middleware is typically custom-configurable and allows a user to program which alarms will be sent to the communication system, the priority of alarms, the nurse or caregiver assignments and the alarm escalation scheme.
The alarm escalation scheme designates which caregiver will receive the initial notification for an alarm, which caregiver receives backup notification if nobody responds to the alarm and the time intervals between each escalation.
Communication devices. Whether they are Voice over Internet Protocol (VoIP) phones or pagers, these are the end devices that are carried by caregivers and are a critical part of an alarm notification system because they directly notify the appropriate caregiver or caregivers.
Video monitors. These are displays that provide visual or audible alarms and alarm information for a variety of devices. Located in strategic locations in the care area, these monitors provide caregivers with alarm notification and specific alarm information.
Design team and its roles
One of the most important tasks a hospital has in the clinical alarm integration selection process is the formation of the design team. Getting the right team together and facilitating multidisciplinary discussion/planning sessions will lead to the selection of an effective alarm integration system and better alarm management, response times, reduced alarm fatigue and improved patient safety.
A good design team comprises both internal and external team members. The internal group should include representatives from the facilities department, clinical engineering (CE), nursing, clinical staff, and professionals in charge of information technology (IT) infrastructure and IT telephones. External participants should include staff from the middleware company that will be capturing alarm information, architects (if the project is part of a new building or renovation), a medical equipment vendor and a communication system vendor.
The CE and facilities departments play a critical role from the outset of any alarm integration system project. Whether part of a new construction project or a renovation, the CE and facilities representatives need to communicate clearly with the hospital's architect. Early on, the architect's team needs to be informed that an integration system is being installed and certain structural considerations must be made — hallways should be designed with backings and cable to facilitate spaces for equipment and monitors in the corridors and walls, and network equipment closets also need to be installed.
Another important role that facilities departments will play is running cabling conduits for these systems. Whether the cables are for video, power or network, they will be required in many areas, including on walls for remote monitors, in hallways for enunciators, or on the ceiling for access points. Making sure these conduits are run may seem expensive, but will be worthwhile in the long run if the system needs to be expanded or if new cabling needs to be installed for other system components.
Like infrastructure, clinical technology is an essential part of designing this system. At this stage, it is critical to seek the whole team's input. The team must decide which technologies will be integrated. Three technologies typically included in an alarm integration system are physiologic monitors, ventilators and nurse call systems.
CE and nursing input also are vital. Because alarm desensitization is an important issue, it is imperative that CE, and the nursing and IT teams come to a consensus on which alarms (e.g., crisis alarms or system alarms such as "leads off") will be transmitted to the middleware.
Additionally, nurses and physicians need to provide input on decisions about incorporating a brief delay in alarm notification so that an alarm is not provided for conditions that resolve themselves quickly. It is important to ensure that the delay will not jeopardize prompt response should the alarm condition not resolve itself.
Hospitals should develop an alarm escalation scheme that is acceptable with their cultures and practices. It should include first-alarm notification, backup alarm notification, and the time intervals that need to be programmed between each escalation scheme.
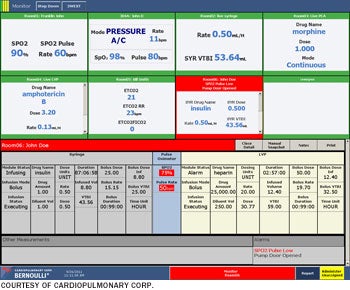 |
| Cardiopulmonary Corp.'s Bernoulli patient dashboard shows summary data of parameters being monitored with such devices as pulse oximetry, capnometry, ventilation and IV pump data. |
IT teams also play a critical part in this process as the need for the network and telephone infrastructure is a key for successful implementation of this system. A proper wireless infrastructure is critical. To avoid missing any alarms on communication devices, there should be no dead zones in the care areas where these systems are being integrated.
Integration of the wireless system, especially to telephony systems, is essential for proper response time. The alarm integration system should be designed based on getting the right information to the right nurse at the right time, and getting the right telephony system is essential.
In most cases this would be a VoIP system. These systems consist of a Session Initiation Protocol (SIP) server. SIP is an Internet protocol that allows for establishing and terminating VoIP telephone calls. VoIP systems also require the installation of an IP private branch exchange server, which registers all VoIP phone numbers and allows a connection to be established.
The external team members also are a critical part in the process of designing an alarm integration system.
The vendors for medical devices identify the alarms and how they are packaged and sent, thus helping the middleware vendors to build the correct bridge to collect these alarms.
The middleware vendors are instrumental in setting up the business rules that will be dictated by the alarm management policies and practices that the nursing team formulates. These business rules then will help parse the alarms to the communication devices effectively.
The communication device vendors ultimately need to ensure that the quality of experience and service provided are on par with the expectations of the clinical team and the internal teams, and that no alarms are being missed.
Five key design areas
Private patient rooms are now the trend when designing new hospitals as they allow for both patient and family privacy. As such, the care areas are increasing in physical size. This creates alarm management challenges and can affect the efficacy of an alarm integration system. To improve the effectiveness and efficiency of alarm notification and response time and to minimize alarm fatigue while propagating alarms to the nurse communication device, the design team should consider the following issues:
Architectural layout. Consider creating zones that are naturally consistent with the floor design. For example, fire doors can be good architectural boundaries that designate one zone from another. Physical distance between the start of the unit and the end of the unit also should be considered as the nurse could be responsible for patients on either end of the care area. Creating smaller, more intimate care areas out of larger areas will create smaller footprints, helping to maintain a reasonable distance to see, hear and respond to any alarms.
Alarm escalation plan. Creating an alarm escalation plan will be easier with clear and consistent divisions between zones. For example, the alarm notification may start with the primary care nurse and then escalate to a buddy nurse. Without a response within a specified period, it would escalate to another designated subset of nurses or all nurses in the zone, thus enabling prompt attention for any patient alarms.
Team coverage environment. Creating practices such as nurse buddies or forwarding alarms to the charge nurse when the primary clinician is busy will allow for prompt attention to any alarms. The key is being consistent with practices, thus improving alarm management and safety as well as creating a better alarm integration system.
Nurse-to-patient ratio and staffing. Consider the staffing ratio for each care area and help determine the number of communication devices needed during peak census. It also may be beneficial to consider adding inventory of these devices to accommodate for shift changes, when some nurses may forget to put their communication devices back. Not having enough communication devices in this model of alarm coverage can lead to inefficiencies in alarm response and jeopardize patient safety.
Technology limitations. A monitoring system may have a limited number of outputs. For instance, there may be a certain number of video outputs if a hospital decides to use video monitors as part of the integration system for visual alarms.
Phone and paging system limitations also must be considered for very large units. These systems can be affected by latencies in alarm notification to the communication devices. This is particularly true in situations with multiple, simultaneous time-sensitive alarms occurring for a larger patient population in a large care area with more nurses.
Some of these issues can be eliminated by looking at the architectural layout and subdividing a large care area into zones. In this scenario, the number of individual alarms will be sent to significantly fewer phones (e.g., eight nurse phones in a zone versus 24 within the care area).
Finally, make sure to test the system to handle the current level of alarms and the anticipated growth in the hospital's size. It also would be advisable to purchase components that are expandable and easily upgradable and invest in the most up-to-date technology that the project's budget can afford.
High-quality care
While integrated alarm systems are not going to reduce the number of alarms that are being generated, they do have the potential to increase the speed at which caregivers can respond because the alarms will be sent directly to their communication devices.
And if a proper alarm management strategy is in place, it can also greatly reduce nuisance alarms being sent to caregivers, because only a subset of the alarms will be sent to them, instead of every single alarm.
Both considerations are important when ensuring the highest quality environment of care.
Rikin Shah is a senior health care solutions engineer for the applied solutions group at ECRI Institute, Plymouth Meeting, Pa. He can be reached atrshah@ecri.org.
| Sidebar - Tech's role in clinical alarm integration |
| Healthcare technology rapidly is fusing clinical and information technology (IT) and a clinical alarm integration system is extremely IT-centric. Indeed, the foundation of these systems is based on proper integration of multiple devices through network infrastructure. There are four areas that should be openly discussed with IT representatives on a project team when planning a clinical alarm integration system. Quality of service. Considerations for ensuring service quality include:
Quality of experience. Considerations for ensuring the quality of experience include:
Validation of the system. Steps for validating the clinical alarm system include:
System support. Measures for supporting the alarm system include:
|
| Sidebar - Testing is key to reliability |
| When a hospital decides to implement an alarm integration system, health care professionals must make sure the system is going to work. Consequently, it is important that they thoroughly test the system to ensure all alarms are received and properly transmitted to the communication devices. Because the system won't be functional until the building is operational, there needs to be a plan to test the system. Testing an alarm integration system is complicated, requires careful planning and must be factored into the design, construction and go-live schedules. The test protocol should simulate the system that will be installed, must include assumptions and decisions that have been made during the planning sessions and should include all the alarm-management strategies. Particularly important is the load-testing simulation, which puts a demand on a system and measures its responses. Load testing looks at the volume of designated alarms that may be transmitted to the middleware and forwarded on to the communication devices. If there are multiple devices that have been integrated into a system, it is essential to determine that the infrastructure put in place can handle the anticipated volume of all the systems simultaneously. Getting the right information at the right time is essential for the success of an alarm integration system. Thus, the middleware also must be tested thoroughly to confirm it is collecting all alarms from the source devices and transmitting the correct alarms with the right priority at the right time. Because the middleware also handles the assignments and alarm escalation schemes, these should be tested to make sure that the alarms are reaching the right person and the escalation scheme is working according to the schedule. If the health care facility has decided to integrate ancillary devices such as ventilators or physiologic monitors to the alarm integration system via a nurse call system, it is imperative that these systems are validated and tested for all types of connections. The systems also should be retested every time any modification or software upgrades have been made. |
