Expanding challenges

When the University of Arkansas for Medical Sciences (UAMS) underwent a major, rapid expansion, acquiring eight satellite facilities over a two-year period, Jonathan Flannery, MHSA, CHFM, FASHE, experienced the growing pains firsthand.
As then-executive director of engineering and operations at the 332-bed academic medical center based in Little Rock, Flannery and his staff encountered challenges on every front — from information technology (IT) and building systems that weren't integrated to a lack of manpower and equipment to an endless series of cost and logistical issues. Then there was the added "windshield time" driving between the central hospital and satellite facilities spread across Arkansas.
"It was quite the struggle," says Flannery, who was responsible for facility assessments for the UAMS expansion from 2010 to 2012 and now serves as senior associate director of advocacy for the American Society for Healthcare Engineering (ASHE). "We were put in the position of making a major transition without having a blueprint in place. We were making plans as we went along."
Sign of the times
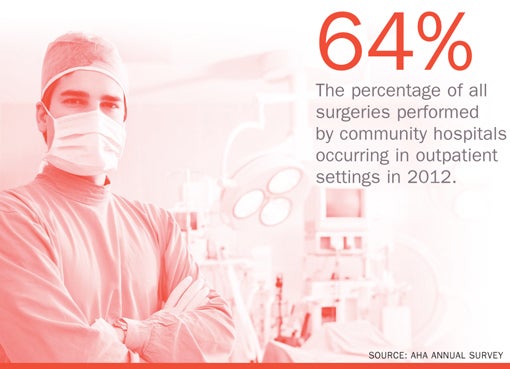
Driven by mandates of the Affordable Care Act (ACA), health care has been moving toward a similar model — a central hospital serving as a hub for a network of satellite facilities — for a number of years. Hospitals working toward ACA goals to expand health coverage, reduce cost growth, improve patient safety and quality of care and expand community-based primary care have been moving quickly to embrace some form of the satellite model since the law passed in 2010.
The transition to a wellness-focused vs. an acute care model is critical as health care moves toward 2014, when coverage begins to extend to an estimated 30 million to 40 million more Americans.
"Hospitals are charged with managing health now as opposed to just caring for the sick; risk has transferred from the payer to the provider's side," says Joseph G. Sprague, FAIA, FACHA, FHFI, senior vice president and director of health facilities for architectural firm HKS Inc., Dallas. "Moving toward an outpatient model is a big part of that culture shift."
Because planning and multidepartment coordination is critical to a smooth transition, department leaders need to be involved in the process from the very first discussion, says Patti Costello, executive director of the Association for the Healthcare Environment (AHE). That involvement is key to helping facilities comply with new Medicare laws that reduce reimbursements for hospitals with high levels of preventable 30-day readmissions.
"Environmental services leaders need to engage in high-level, strategic discussions with their peers and within their own organizations about how the wellness focus will shift inpatient care to the sickest patients and how that shift will impact the operation in terms of measuring outcomes, preventing readmissions and improving Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores," Costello says.
Adds Flannery: "Hospital systems tend to look on this type of a transition from the clinical aspects and the support side as almost an afterthought. Facilities managers need to be in on these discussions from the very beginning; that is critical to a smooth and successful transition."
Surmounting setbacks
Experts point to the many advantages hospitals stand to reap from the transition — from sharing expertise among buildings to cost savings tied to bundling services — but say getting to that point is fraught with challenges, especially considering the looming reform law deadlines.
One common difficulty is restructuring of staff, which can present a difficult adjustment for some managers. "Facility managers tend to function autonomously, so it's a big change when they are asked to expand their focus from one building to multiple facilities," Flannery says.
And because most hospitals are adapting existing buildings, those facilities also come with existing problems. At UAMS, one facility was donated to the network, but needed all new infrastructure — chillers, boilers and generators — which set the hospital back millions of dollars. "This is common since many of the facilities acquired were already struggling, and support services and infrastructure maintenance tend to be some of the first things that get cut," Flannery says.
And there were other setbacks. When UAMS purchased a facility that had been shuttered, Flannery was asked to get the building up and running with no additional staff. "That would mean taking staff from the central facility, which we were just not set up to do," he said. "It's ultimately about evaluating staff and weighing the best use of their time. In this case, we realized it made more sense to contract the work out to get the facility up and running."
Costello says multifacility systems often place a contract team in one building and an in-house team in another. "You need to figure out which model is right for each building — or system," she says.
Determining the best use for each facility is also critical to the outpatient model. Sprague says patient-focused designs should feature clear access points, allow the coordinated flow of patients through the building, and maximize safety and quality of care.
And, as facilities become interconnected and standardized across networks, branding will become a bigger part of the design strategy as well, Sprague adds. "There's much less fragmentation, so you want continuity from building to building."
Importance of interconnectivity
Technology is always a top priority, considering that interconnectivity is critical among multifacility systems.
At UAMS, for example, satellite facilities were equipped with different operating systems, "so we ended up learning how to operate three or four building automation systems," says Flannery. He adds that staff also are using email to communicate between buildings until the system is standardized. Flannery advises hospitals to "maximize the knowledge of staff who are most expert with systems controls" and assign them to work throughout the system.
While connectivity of patient data through electronic health records (EHRs) is also critical, Thomas Skorup, FACHE, vice president of applied solutions, ECRI Institute, says "maintaining a consolidated EHR across a patient's continuum of care becomes more challenging with more discrete patient data acquisition sites."
One solution: Health information exchanges that instill a central broker for coordinating access to patient health information, helping hospitals to achieve meaningful use objectives and improve patient outcomes.
Satellite facilities should be equipped with a robust Health Insurance Portability and Accountability Act-compliant wireless local area network, and user interfaces will need to accommodate less sophisticated users in a community setting, Skorup says. Hospitals need to expand equipment management programs to include satellite facilities that own medical equipment and should conduct an initial equipment inspection and possibly ongoing preventive maintenance checks, he says. "A lot of times, equipment at satellite facilities falls through the cracks," Skorup adds.
On the supply side, multifacility systems are challenged to properly integrate supply chain data across all of the facilities, says Kayla Sutton, Economic Outlook managing director at Premier Inc.
"Integration of supply chain and clinical data can be achieved in health systems' EHRs, but advanced data analytics aid in making data actionable," Sutton says. "Supply chain integration to align with clinical care, revenue capture and IT across all facilities within a health system is the second biggest trend impacting supply chains in the next 12 months, and it has risen 9 percent over the last six months."
Health systems increasingly are implementing centralized purchasing channels across all of their facilities to better manage supply expense across their expanded provider networks and drive supply chain savings, Sutton says.
Advantages abound
Although the prospect might seem overwhelming, managers who have successfully navigated such a transition say it's important to realize the model is not only attainable, it's advantageous. "This isn't something new," Flannery says. "Catholic Health Initiatives and other health systems have been doing this successfully for decades across many states and regions."
Flannery says decentralization offers a number of benefits across the health care continuum. UAMS was able to build an economy of scale by bundling contracts for waste, water treatment, fire alarm and other services into the central hospital's existing contracts, cutting costs significantly. Hospitals also are able to share the expertise of staff members — a big plus for smaller facilities with a leaner staff. Smaller facilities can benefit from the safety, recycling, energy and regulatory programs in place at the central hospital. Due to its small size and rural location, one of the UAMS satellite buildings had no recycling program in place. "As with many other programs, we rolled it into ours, which is a huge benefit to them."
And despite the numerous obstacles, Costello says the outpatient model offers managers a real opportunity to demonstrate their value — especially since streamlining and consolidating operations can lead to big cost savings.
"Managing multiple buildings is difficult and challenging enough, and creative managers who are able to juggle the competing demands of inpatient and outpatient unique infrastructures, staff cultures and equipment, are saving their organization time and money; and in the end, valuable resources go right back into the excellence of care across the entire continuum," Costello says.
And that value extends to the patient — exactly as health care leaders intended, Sprague says.
"I think most hospitals and networks are optimistic about this model and the accompanying changes," Sprague adds. "It's their mission to take care of people and have a healthy community, and these changes tie into that."
Beth Burmahl is a freelance writer based in Oak Park, Ill., and a former associate editor of Health Facilities Management.




