Measuring and controlling greenhouse gas emissions

Facilities managers should start with the basics that include tracking usage and making sure systems are working correctly as well as proactively implementing capital expenditure plans.
Image by Getty Images
Sustainability, decarbonization, carbon neutral and net zero are becoming part of the health care vernacular and have been seen and heard via American Society for Health Care Engineering conferences, websites and publications.
But what do they mean for health care facilities management? Why does a health care organization need to be concerned? More critically, how can facilities managers and directors be a part of the effort to bring these terms to realization?
The facility’s role
Starting at its core and going beyond politics, climate change caused by greenhouse gas (GHG) emissions threatens the health of the planet and, ultimately, human health. Because patient care is a fundamental rationale for organized health care, health care organizations must address the health care facility’s role in climate change effects.
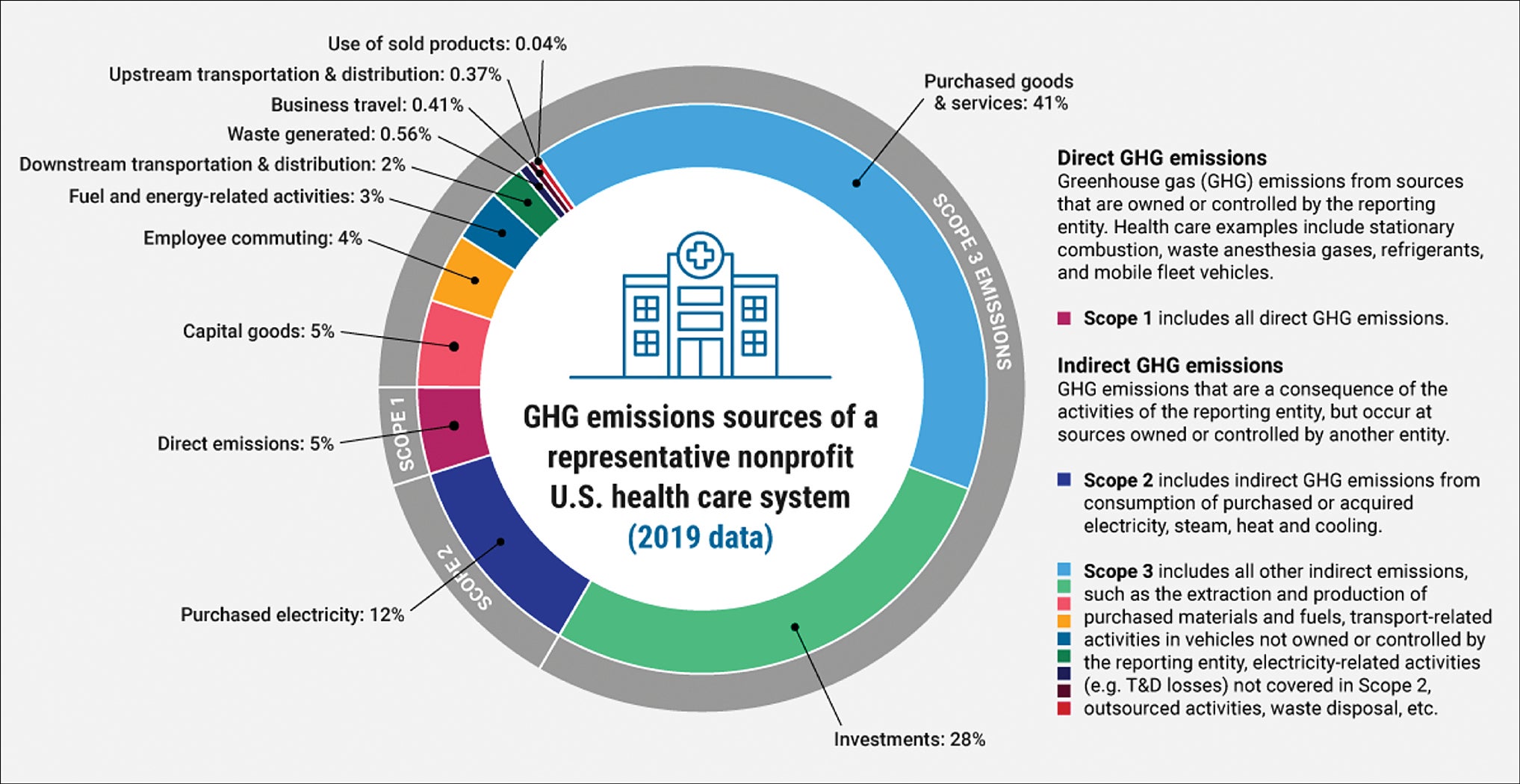
Accounting for 8.5% of the nation’s carbon emissions, health care facilities carry an obligation beyond regulatory compliance that is foundational to the health care provider’s mission and operations. One of the guiding frameworks of emissions reduction is driven by the GHG Protocol of identifying and categorizing each emission by scope, which can be accessed at ghgprotocol.org.
Scope 1 emissions are produced from facility operations. Typically, the largest Scope 1 contributor from a facility is power generation, such as from the combustion of fossil fuels from boilers and generators. Smaller in volume but greater in impact are leaking refrigerants and anesthetic gases, such as nitrous oxide. Additionally, emissions from hospital-related transportation or fleets that use fuel contribute to these emissions.
Scope 2 emissions are from the energy consumed from purchased utilities or steam that operate the facility. These account for about 18% of the facility’s GHG emissions, leaving the largest scope to the supply chain, or Scope 3, which encompasses the production, distribution and disposal of goods and services such as embodied carbon in medical supplies, building products, pharmaceuticals, food and waste. Scope 3 also includes transportation of staff, vendors, visitors and patients (see the graphic below).
Much of the terminology regarding climate change and emissions reduction has been evolving as the movement to decarbonize systems has progressed. What was once a warning about global warming is now a call to action to mitigate the effects of climate change, which are causing variations in temperatures, water levels and extreme weather events. “Carbon neutral” has been a common term referring to lowering carbon dioxide (CO2) emissions through energy reductions and purchasing carbon offsets, such as planting trees or carbon capture, or investing in renewable energy. But the term that is at the forefront of climate pledges and commitments is “net zero,” which goes a step further than carbon neutral. Net zero incorporates all GHGs, including not only CO2 but other gases such as methane, hydrofluorocarbons, perfluorocarbons, sulfur hexafluoride, nitrous oxide and nitrogen trifluoride, and requires organizations to reduce their production across their entire supply chain. While CO2 mitigation is still the primary driver of net zero goals, addressing non-CO2 GHGs through demand reduction, fuel switching, or choosing alternative refrigerant or anesthetic gases in the hospital environment are critical.
Policy drivers
Significant changes in federal, state and local policies and initiatives have driven the need to set emissions reduction targets. In 2022, the Department of Health and Human Services created the Office of Climate Change and Health Equity, which then implemented the White House Health Sector Climate Pledge, which dictates health care system signatories to reduce their facility’s emissions by 50% in 2030 and achieve net zero by 2050.
As of November 2023, more than 133 health care-related organizations representing over 900 hospitals have signed the pledge. Implementation of these targets has been aided with the Inflation Reduction Act’s tax credits and direct pay provisions for renewable energy and energy efficiency projects. Meanwhile, other organizations such as the National Academy of Medicine, American Hospital Association and The Joint Commission have created roadmaps and certifications encouraging health care organizations to implement decarbonization programs.
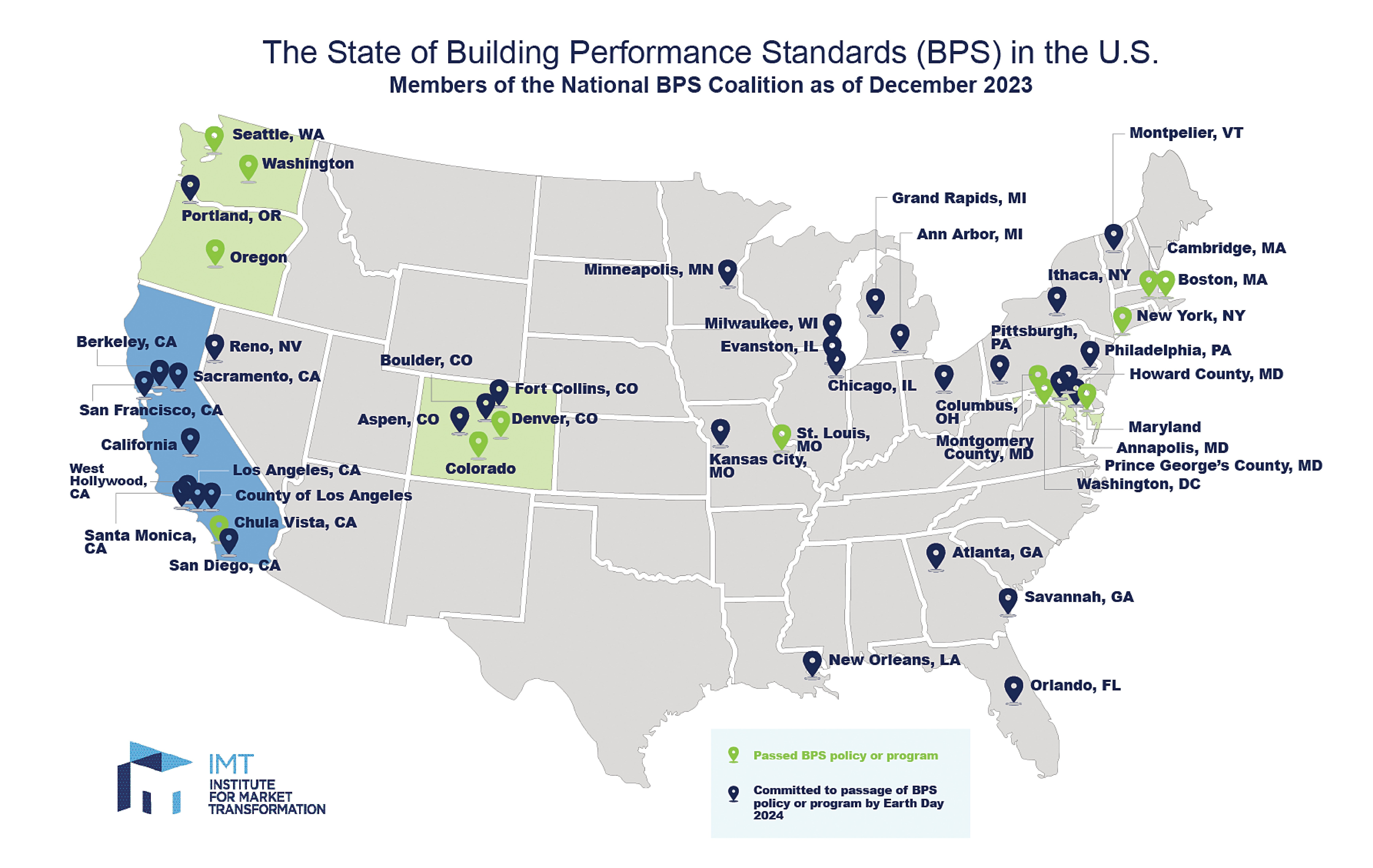
Health care facilities across the U.S. have also been greatly impacted by new building performance standards (BPS) implemented mostly with new state and city policies (see the graphic below). These BPS can vary but typically incorporate some emissions reduction targets within a certain time frame and penalties if they aren’t achieved. For example, the city of Denver implemented a building decarbonization policy that applies to commercial and multifamily buildings 25,000 square feet and larger. It requires each building to meet a maximum site energy use intensity (EUI) standard based on its occupancy type by 2030. Using benchmarking tools from the Environmental Protection Agency’s (EPA’s) ENERGY STAR® program, building owners must submit an annual benchmarking report indicating their improvements in EUI and track performance. Failure to act can result in fines and penalties from the city of Denver.
In March 2022, the U.S. Securities and Exchange Commission proposed rules that would require reporting companies to provide data related to climate change in their registration statements and annual reports. This data includes Scope 1, Scope 2 and, if material, Scope 3 GHG emissions. While the final ruling has not been made, the impacts on health care facilities would include the disclosure of GHG emissions and climate-related risks that could disrupt care or damage facilities, and governance and risk management to plan for climate-related risks.
Calculating and reporting
Calculating and reporting GHG emissions has often been perceived as a complex endeavor. Organizations grapple with decisions on what to include or exclude, which emissions factors to employ and how to update and report annually. Fortunately, standardized practices and tools exist to simplify this process. The GHG Protocol supplies the world’s most widely used GHG accounting standards. It provides comprehensive guidance, tools and training available for use, much of which is accessible at no cost. Prior to embarking on reporting emissions, organizations are strongly advised to acquaint themselves with the GHG Protocol corporate accounting and reporting standard to minimize calculation and reporting mistakes.
Once familiar with the concepts for reporting emissions, an organization can use either a simplified GHG emissions calculator available through the ENERGY STAR Portfolio Manager or other third-party tools available to calculate the facility baseline and reporting period GHG emissions. The EPA provides an Excel file version of the calculator tool and guidance at epa.gov/climateleadership. When opting to use a third-party tool, the provider should ensure the tools are consistent with the GHG Protocol corporate standards approaches.
Many organizations are familiar with ENERGY STAR Portfolio Manager and use the tool to track energy consumption and energy efficiency progress. The building emissions calculator expands on the existing Portfolio Manager’s GHG emissions capabilities and leverages an organization’s existing Portfolio Manager data. The building emissions calculator allows users to create location-based and market-based GHG emissions estimates, apply historic emissions factors to prior years’ energy consumption and forecast emissions based on a set of user-defined assumptions.
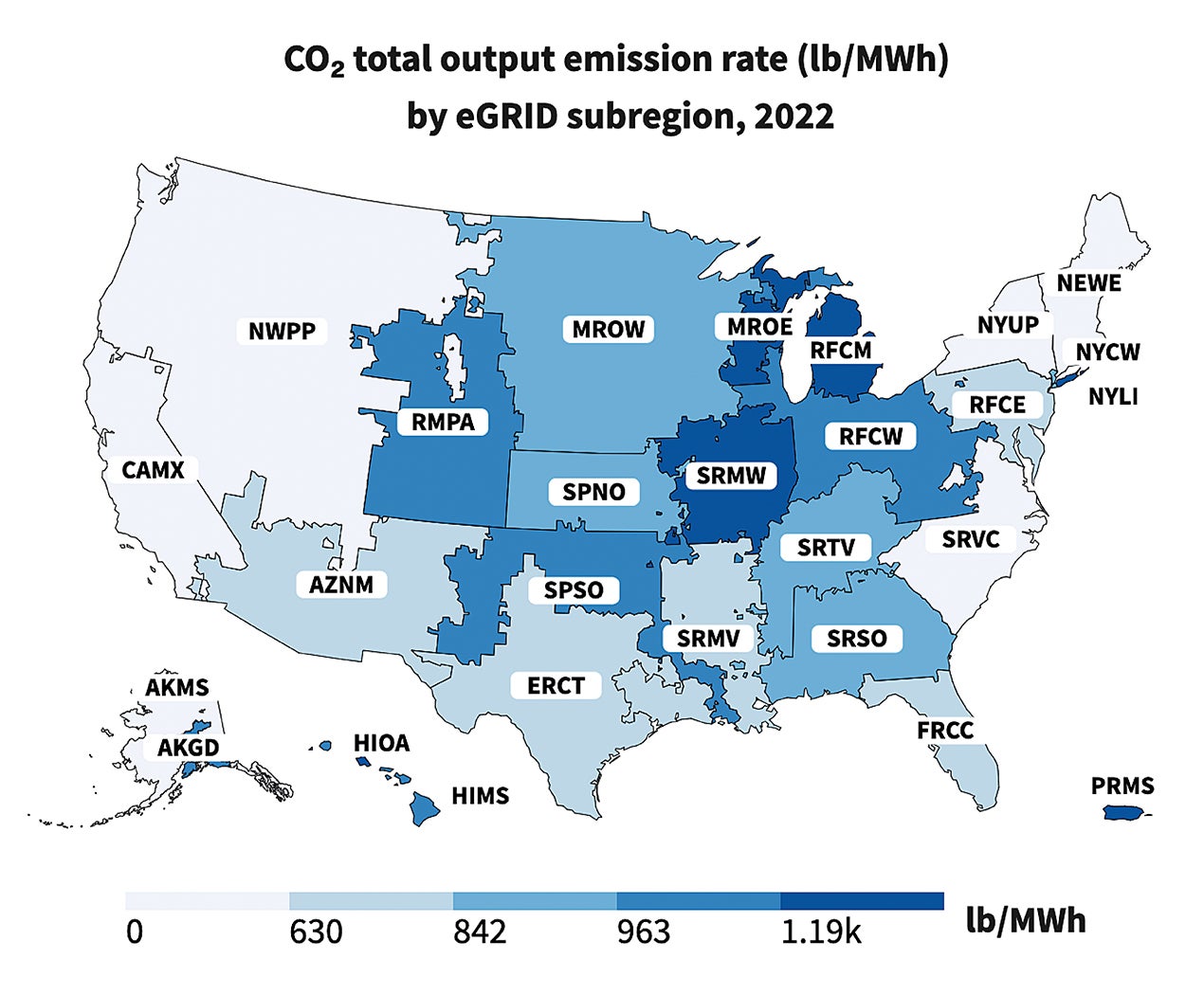
The utility or supplier that serves an individual facility plays an important role in that facility’s GHG emissions and its reduction strategy impact. Scope 2 (e.g., electricity) emissions vary across utilities and regions (see the graphic below).
Each utility has a different generation mix that affects emissions factors. When analyzing an individual facility’s GHG emissions associated with electricity consumption, it is important to know the current, historical and projected emissions factors for the electric utility serving the facility. Most utilities have an integrated resource plan with projected GHG emissions for future years available on the utility’s website, which may include the utility’s GHG emissions reduction goals. An organization should take each utility’s GHG emissions reduction goals into account when addressing each facility’s emissions calculations.
While Scope 1 (e.g., fuels, refrigerants and gases) emissions may seem straightforward, it’s crucial to consider things such as default emissions factors provided by the EPA and any separately calculated emissions factors from suppliers. The EPA’s website offers annually updated default emissions factors by source that can be used for GHG emissions calculations. The supplier may have separately calculated emissions factors for the product they are supplying. If so, they should be used in place of the EPA default values.
When publicly reporting GHG emissions, there are some basic practices that should be deployed to ensure complete, transparent and accurate reporting. An organization should set organizational and operational boundaries that ensure complete reporting of relevant emissions inside those boundaries. This means that the information being provided is needed for decision-making.
It’s important that the reported information is meaningful. While reporting Scope 1 and Scope 2 emissions is required for many programs and climate pledges, Scope 3 emissions accounting is mostly optional. Identifying relevant Scope 3 emissions to include in reporting is an important step. There is guidance for identifying Scope 3 emissions available for health care organizations from the National Academy of Medicine and Health Care Without Harm.
An organization must ensure business goals for reporting GHG emissions have been clearly defined and adequate resources are allocated to provide consistent reporting to meet those goals. Managers should make sure processes for collecting, maintaining and auditing data are established to track emissions over time. They should document the methods, assumptions and estimates used in all the calculations and implement quality checks. Metrics should inform and show the progress toward the organizational goals. While the primary metric is the overall impact on GHG emissions, metrics like GHG emissions per square foot may demonstrate progress during periods of growth. A successful reporting strategy is vital for GHG emissions reduction.
Carbon reduction strategies
Reducing carbon emissions can be challenging, especially in a hospital, which is one of the largest producers of carbon per square foot compared to other buildings. However, this also presents more opportunities for improvement. The most important objective is to start with the basics, including tracking usage, making sure systems are working correctly and proactively implementing capital expenditure plans to replace aging infrastructure. These tasks focus on Scope 1 and Scope 2 emissions. This involves:
- Tracking energy usage by building and determining EUI. Managers should establish an account for ENERGY STAR Portfolio Manager to report the facility’s numbers. This allows the facility to be compared to peer facilities and assists with identifying buildings that have the most potential for reducing energy and emissions. Adding electric submetering may also be necessary.
- Embracing commissioning on new projects and implementing extensive retro-commissioning plans on existing facilities. This will identify functional issues, such as unintended simultaneous heating and cooling, unutilized setback opportunities, excessive reheat use and others. This has produced surprising results. Large health care campuses implementing retro-commissioning plans have seen energy reductions of over 30%.
- Being proactive about developing and proposing annual capital expenditure plans to the C-suite. This is necessary to replace aging infrastructure. Such projects include upgrading to more efficient central equipment, LED lighting and modern control systems. Again, retro-commissioning will assist with developing the list.
Managers must understand the direction the field is going to further reduce energy and carbon emissions for new projects. They should explore opportunities to implement renewable energy and solar by leveraging grants and tax credits. They can also consider designing new roof areas to add photovoltaics in the future, even if it is not viable for a current project. They should engage local utility companies and other energy partners to purchase renewable energy credits or partner to construct solar fields at an off-campus site.
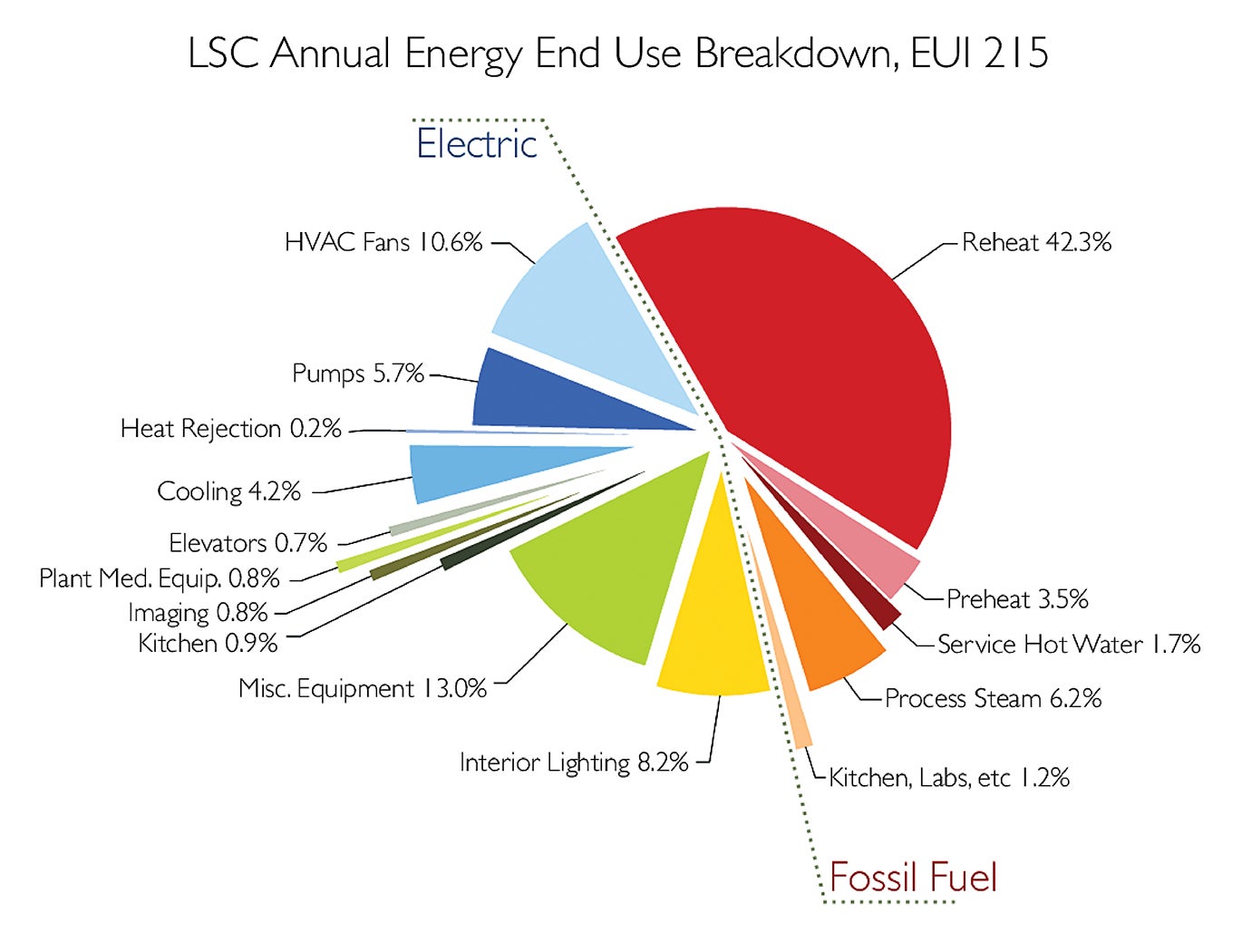
Reheat energy accounts for the largest percentage of energy used in a hospital, regardless of location (see the graphic above). Heating systems are a big target for reducing energy, as they typically account for over 40% of a hospital’s energy use. This will require migrating away from using steam. Point-of-use steam generators, separate low-temperature heating water systems and atomizing technology for humidification are methods of reducing traditional steam use.
Heating, ventilating and air-conditioning equipment manufacturers are currently investing in heat pump technology, which is a critical element to reduce energy and pursue electrification goals. Heat pumps work well with low-temperature heating water systems and heat recovery systems. They are two-and-a-half to four times more efficient than gas boilers or electric resistance heat. Expect heat pump technology to continue to improve.
Driving change
The U.S. health care field has always been a world leader. Coming together to address climate change is an impactful way to benefit the health of its patients.
With new tax credits, incentives and grants, now is the time to understand an organization’s impact on emissions and develop plans that can save money and create more sustainable and resilient facilities.
Answering the emissions challenge
Health care is tasked with being part of the solution to improve public health by countering the effects of global warming and improving the quality of the environment. The pressures in society to lower energy consumption and emissions in health care are profound and increasing every year. This is derived from legislative actions, environmental awareness, challenges to replace diminishing resources and demands from the international community to curb climate change.
Accepting the inevitable is the important first step to recognize and acknowledge that the health care field must improve. This is especially true considering the disproportionate contribution health care facilities make to emissions compared to other building types. The following questions are likely some of the first ones that come to mind:
- What are emissions?
- How are energy and emissions related?
- How does a health care facility contribute to emissions?
- How are emissions measured?
- How can emissions be reduced?
The objective is to achieve a better understanding of these questions and how to align the answers to a specific facility. Reducing emissions is a complex subject and an endeavor that will take many years and advances in technology to make substantial progress. However, making impactful progress is well within reach today.
With a clear understanding of where a facility is today and where managers want it to be in the future, a facility can take the next steps to investigate and implement strategies to reduce emissions. Factors such as costs, feasibility, timeline and financial return should be considered to prioritize initiatives.
An effective measurement and verification plan is critical to monitoring the success of initiatives. However, this plan can also assist with determining where the biggest opportunities exist by identifying buildings that produce the highest levels of emissions per square foot.
Developing a culture of awareness and improvement will yield long-term success. This will allow the facility to be recognized in the community as a leader in sustainability.
Jessi Bienert, CEM, is vice president of sustainable solutions at Bernhard LLC, Metairie, La.; Kathy Henderson, CEM, is a national business development manager for health care at Ameresco Inc., Birmingham, Ala.; and Scott Winfrey, PE, HFDP, LEED AP, is associate principal at Specialized Engineering Solutions, Omaha, Neb. They can be reached at jbienert@bernhard.com, khenderson@ameresco.com and swinfrey@specializedeng.com.