Mitigating Legionella with a targeted response
Hospitals can maintain safety by incorporating clear and targeted procedures for sampling and understanding causes of Legionella bacteria growth.
Image by Getty Images
When faced with a possible infection risk from Legionella colonization within a hospital water system, many health care systems take broad, buildingwide actions to stop the risk before it spreads, and they will continue to repeat those same actions without understanding the root cause.
Common recommendations are to periodically add chlorine disinfectant (either low-level or a “shock” chlorination) to a water system or install a secondary treatment system. However, these solutions are not always necessary, can be expensive to implement and disruptive to critical operations. What’s more, these broad actions are not always effective in mitigating the risk.
When facilities managers approach Legionella issues by first identifying the source or cause of system colonization, they are often able to successfully mitigate the risk of Legionella with targeted solutions. These more targeted actions can often be more focused on the major causes compared to buildingwide and systemwide actions and, ultimately, can be far more effective.
Systemwide treatment may be needed, but without having a proposed explanation or a known source, these solutions simply may not work. By incorporating clear and sometimes very targeted procedures for sampling within a water management program and understanding and mitigating common causes of Legionella bacteria growth, hospitals can effectively keep their populations safe.
Identifying the risk
The Centers for Medicare & Medicaid Services requires that hospitals have a water management plan in place to mitigate the risk of Legionella and other waterborne pathogens. This requirement is now joined by The Joint Commission’s new water management program standard (EC.02.05.02, EPs 1 through 4), which establishes a framework for developing such a program.
These entities agree that a key component within any water management program is the ability to gauge its efficacy through a monitoring program. This monitoring should include the routine measurement of potential risk conditions.
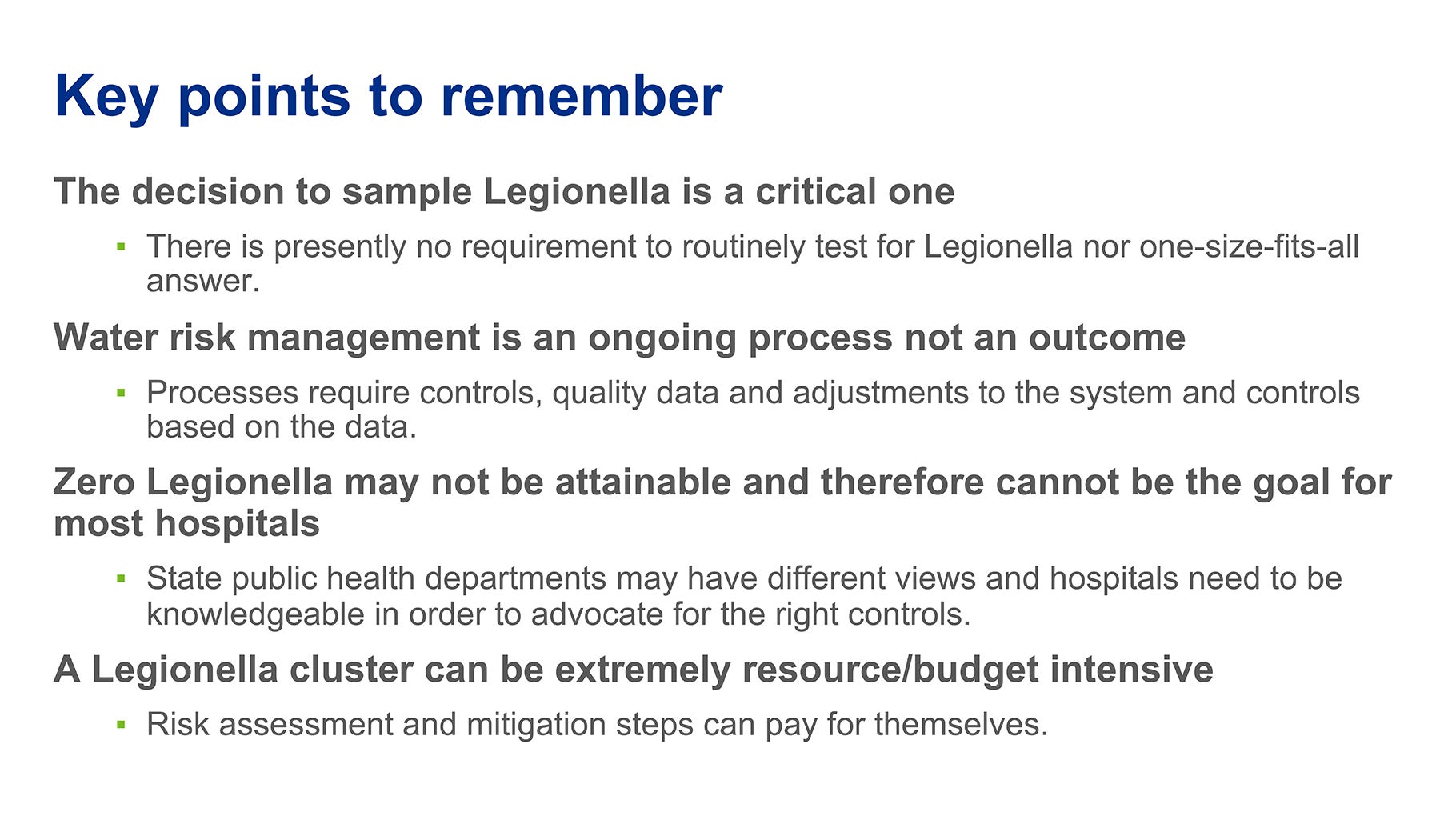
These measurements may, but do not have to, include measuring for the presence of Legionella bacteria. In fact, it’s up to individual health care organizations to determine whether to monitor directly for Legionella within their water systems. While it may seem counterintuitive to not screen directly for Legionella bacteria itself, sampling for “screening-level” parameters can be a very effective gauge as to whether conditions are ripe for bacteria growth at levels that create risk for potential infection.
Why? Low levels of Legionella bacteria can be found periodically within most complex water systems. Should testing identify the presence of Legionella within the water system, the reflexive action is to try to eliminate the presence of the bacteria to achieve zero colony-forming units, often through the costly and sometimes ineffective interventions discussed previously. Yet, because Legionella is a naturally occurring bacteria and can often present in low levels in complex water systems such as in hospitals, achieving this level-zero goal 100% of the time is not often feasible and, most importantly, periodic and low-level detection of Legionella does not necessarily indicate an elevated infection risk.
Maintaining as low a percentage of Legionella as possible is certainly an ideal goal, but there are other parameters (along with percent positive) that, when taken together, are a better gauge of risk. Among these would be an upward trend in positive samples over time that can provide clear evidence of bacterial growth and system changes.
In addition, the presence of Legionella pneumophila serotype 1, as compared to other forms of Legionella, should be a cause for further investigation. This particular species or serotype is responsible for over 85% of infections with Legionnaires’ disease, which has a fatality rate of up to 10% in the general population and as high as 40% to 80% in untreated immunosuppressed patients, according to the World Health Organization’s “Legionellosis” webpage.
Screening parameters
Rather than testing specifically for Legionella, facilities managers may find it useful to measure screening parameters that are indicative of conditions conducive to bacterial growth. For health care facilities, the most common such parameters include the following:
Residual disinfectants. This is typically a chlorine product used by water treatment plants to limit the growth of Legionella and other waterborne pathogens. Measuring the amount of residual disinfectant at dead-end fixtures within a facility can help facilities managers determine the effectiveness of this disinfection as it moves from the water treatment plant to the local facility.
The key is understanding what is being monitored, what the result means and agreeing to a range of actions if results are out of the accepted range. This begins with determining the type of disinfectant the municipal water system uses. There are a few types of chlorine-based disinfectants that may be used and the differences among them will impact monitoring methods and the expected measurement results.
It is important for a facilities manager to understand the primary and secondary disinfectant from the public water supply and therefore be able to set the correct ranges at the outlets in patient rooms and other areas of the hospital.
Temperature profiles. Keeping cold water cold and hot water hot is a critical step in limiting the potential for Legionella and other waterborne pathogens’ growth. As such, temperature profiles can evaluate whether conditions are healthy or present a risk.
Temperature profiles track how hot the water gets and how long it takes to achieve maximum heat. Achieving peak heat should happen within 60 to 90 seconds. Hot water that takes 3 to 5 minutes to reach peak heat may be an indication of the stagnant water in which waterborne pathogens thrive.
Monitoring the temperatures throughout the hot and cold water loops to ensure these stay within the established temperature ranges is an important control measure.
Total heterotopic bacteria. Rather than measuring Legionella directly, this is a measurement of essentially all bacteria present as an indication of the potential water contamination risks. After all, Legionella is hardly the only waterborne pathogen that can cause infection. However, it is important to note that total heterotopic bacteria is measuring all bacteria, not just pathogenic ones, and therefore should only be considered a “screening level” parameter.
A sampling strategy
Knowing what to sample is an important first step, but it’s also important that sampling be conducted within context provided by a clear sampling strategy. To begin, sampling should be performed to answer specific questions. For hospitals performing proactive sampling for Legionella, the question might be as simple as asking, “Are we maintaining consistently low levels of Legionella?” An investigation into a potential infection risk might ask, “Where are possible sources of Legionella?”
To find the answer to these questions, facilities managers might traditionally have sampled for Legionella in patient room fixtures, showers and other water outlets. While this is a good approach for a proactive assessment and can identify that a problem is present, it may not narrow the source of the bacteria once colonization is suspected based on elevated results or during a patient infection investigation.
A forensic sampling approach is a more useful alternative or addition to the traditional approach, during a time when water system colonization is suspected. This involves selective, targeted water sampling for Legionella focused in areas where sources may be suspected.
For example, sampling of hot water tanks or water directly downstream of hot water tanks can help assess the hot water systems’ influence on elevated results. Also, water sampling in selected access points in the water systems, rather than sinks in patient rooms alone, can also be a useful forensic tool for locating stagnant areas of water. By narrowing down the area where the problem originated, facilities managers can develop a more focused, effective mitigation plan.
To ensure the effectiveness of this approach, it’s important to have a strong understanding of a campus and plumbing system. Facilities managers may already have suspected trouble areas in mind and this can help guide the sampling strategy.
Targeted treatment
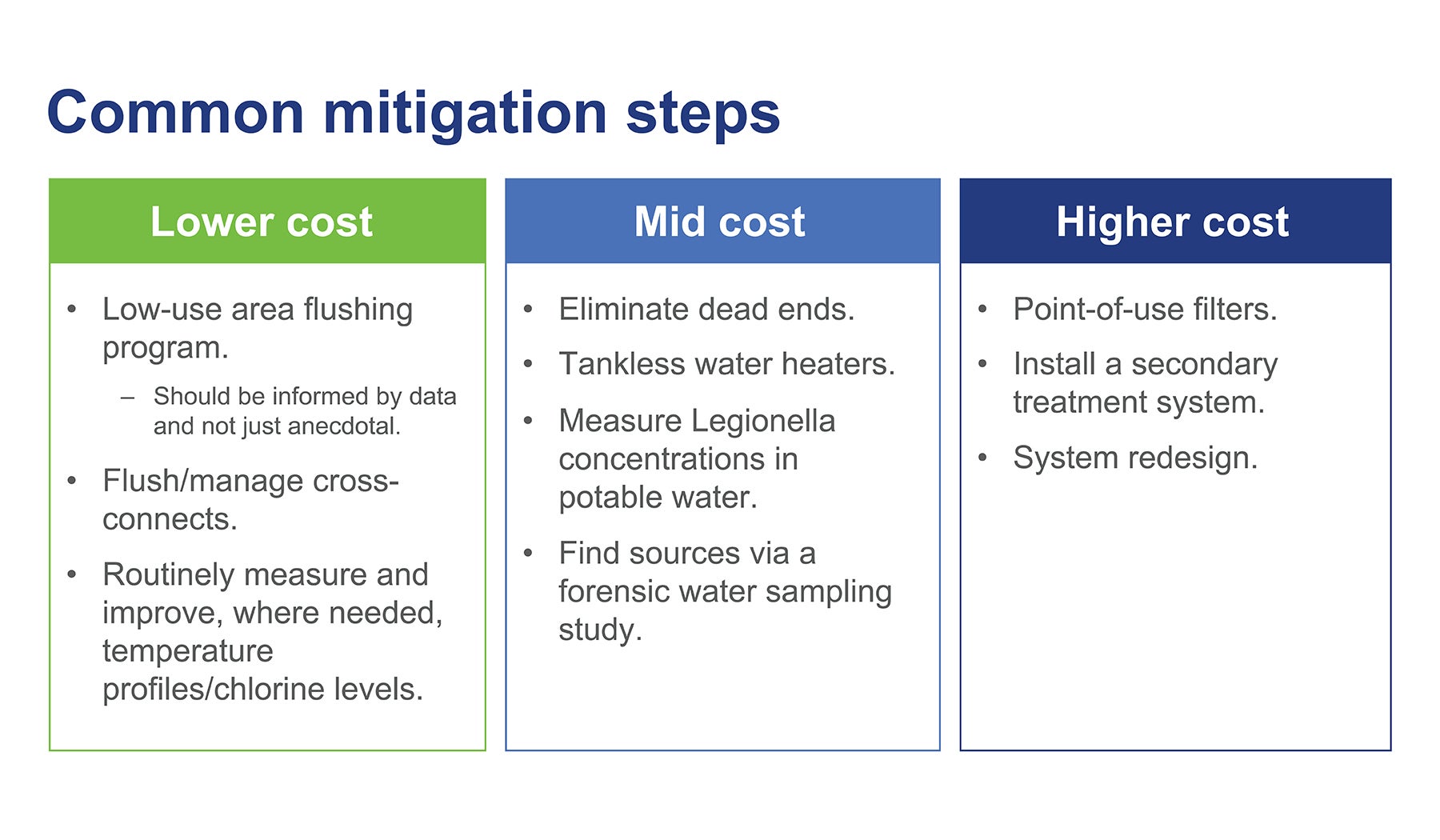
Once the source has been identified, facilities managers can plan a targeted response that is likely to require a simple, low-cost solution. A few such options include the following:
A flushing program to eliminate stagnant water. Flushing is best performed when there are a discrete number of locations indicating a possible local issue with Legionella. For example, if only one or two floors within a multistory building present evidence of Legionella or low levels of chlorine disinfectant, flushing may be a good solution. When a small percentage of locations present this problem, it’s typically evidence of one or more local issues, many of which can be addressed. Perhaps the impacted floors have more dead legs in which water has been able to sit, or there is a problem with the hot water recirculation system serving those floors. Perhaps the areas have increased “water age,” as the location is furthest from the point where water enters the building and is therefore stagnant longer and loses its residual disinfectant.
Before beginning a flushing program, facilities managers should take time to collect data to guide the process. A real-time chlorine measurement is a useful way to ensure that a flushing program is driven by data. Because the level of chlorine in the impacted area is an indirect way of measuring how stagnant the water is, this metric can help determine if flushing is the right approach.
Maximize effectiveness of hot water heating and distribution systems. Because Legionella grows best in environments that maintain a temperature range between 77 F and 120 F, it is important to maintain a consistently cold or hot water temperature as the system demands.
Of course, there are several factors that can impact the delivery of hot water throughout a hospital. Potential issues may include insufficient hot water temperatures at the heater, uninsulated lines, dead ends of pipe within the hot water system or booster pump failures that prohibit hot water from effectively traveling from the mechanical room to the highest floors of a facility.
Facilities managers should consider having a qualified engineer evaluate the potential for these types of issues during hospital assessments to help proactively prevent many of these problems.
Develop management strategies for cross-connects. Large hospital campuses may have one or more cross-connects linking buildings across campus. These pipes allow for redundancy in water distribution across multiple buildings in case of failure in one building’s water system. The challenge is that this rarely used section of pipe can become a location where water stagnates.
The good news is that because these sections are known, there are important steps that can be taken to prevent stagnation. A proactive flushing program can push water through the piping perhaps once or twice a month, as laid out in a water management program.
Elimination of dead ends. Whereas a campus might have a few well-known cross-connects, dead ends can be more complicated. In some cases, these pipes are left over from a renovation or a placeholder for a future expansion. The bottom line is that they are often hidden, difficult-to-access locations where water can stagnate.
Ideally, facilities managers will want to identify and proactively eliminate as many such sections of pipes as possible by tracing their system. However, if an issue hints to the presence of dead ends, it’s a good idea to perform a selective investigation within that area by opening the wall with a few targeted cuts.
Systemwide treatment
With a well-planned investigation, facilities management and infection control and prevention teams, working with consulting experts in water management (industrial hygienists and engineers) can typically uncover the cause of Legionella colonization and take appropriate action to mitigate this risk. However, there are rare instances where hospitals may deem that a bigger solution is necessary, such as a water treatment system.
Full-scale water treatment systems are meant to be a last resort for facilities that can’t readily identify the source of their waterborne pathogen risk. For example, these secondary treatment systems may be useful on campuses with broad Legionella risks across multi-age buildings.
However, there are major challenges that come with these systems. First and foremost, secondary water treatment systems can be incredibly costly. A full cost analysis should be conducted to determine first costs as well as ongoing maintenance costs before taking this step. In addition, such systems may require a permit to implement. With their operation, hospitals may find they are essentially operating a water treatment facility on their campus.
If a treatment system is determined to be necessary, it is important to identify upfront the potential impact it may have on the facilities’ plumbing systems. For example, solutions like sodium hypochlorite injections or monochloramine treatments can contribute to corrosion in plumbing system pipes, joints, fittings and fixtures over time, and chlorine dioxide treatments can damage polyethylene pipes.
Moreover, these solutions may not always be effective in penetrating established biofilms or controlling Legionella associated with such biofilms. As a result, it is important that secondary disinfection systems only be installed as part of a comprehensive water management program that addresses all facets of these risks.
The American Society for Health Care Engineering’s monograph “Water Management in Health Care Facilities: Complying with ASHRAE Standard 188” provides a listing of the advantages and disadvantages of treatment options in its Appendix 1. It can be accessed via the ASHE Resource box on this page.
Well-planned program
A facilities manager’s first line of defense against waterborne pathogens is a well-planned water management program that includes clear parameters for monitoring water systems for risk.
While it takes time and effort to develop a useful, comprehensive plan, it’s far better to take those steps today.
Should an infection occur, or a state public health department thinks one may have occurred, those steps will still be required but under the surveillance of state and federal public health officials.
With advanced planning and a clear understanding of screening parameters, facilities managers can proactively mitigate the risks of both Legionella and unnecessary operational downtime.
A case study of an investigation into a hospital Legionella outbreak
After two patients tested positive for Legionella within six months of one another — including one who spent 18 days in the hospital before testing positive on day 19 — a hospital was faced with an intensive nine-month environmental investigation with a state public health agency.
Water sampling for Legionella returned 60% positive samples with ranges from non-detect to approximately 150 colony-forming units per milliliter of water, identifying the hospital as the most likely source of the infections. To contain the risk, the facility installed point-of-use filters. However, filters couldn’t eliminate the risk entirely, so the facility began a forensic study to uncover the source of the bacteria.
Environmental sampling, as indicated by the environmental assessment, focused on several key areas, including:
- Incoming water. Sampled during and after a flush, this helped characterize Legionella sources within the facility as related to incoming city water.
- Hot water recirculation loop. Sampling upstream and as close as possible to the instantaneous hot water heaters and heat exchangers helped quantify Legionella sources related to the hot water piping and recirculation loop.
- Hot water supply. Sampling at and directly downstream of each instantaneous hot water heater and heat exchanger characterized the potential for Legionella growth related to these sources.
- Hot water at outlets. Running hot water from several outlets for several minutes to effectively use up the volume of recirculated hot water in the loop helped characterize Legionella sources related to incoming water heated once through the hot water heater. Legionella found here is often attributable to the hot water generator system rather than system piping.
The investigation uncovered stagnant water within dead ends that were eliminated near the water heaters and biomass formation near water hammer arrestors, as well as contaminated aerators on two floors.
Water sampling continued every two weeks throughout the investigation until the risk was determined to be mitigated. All told, the reactive study cost the facility more than $600,000 in sampling, system modifications and point-of-use filters.
About this article
This article is based on a presentation by the author during the American Society for Health Care Engineering’s 2022 ASHE Annual Conference in Boston.
Bryan Connors, CIH, HEM, is managing principal consultant for health care at Environmental Health & Engineering Inc., Newton, Mass. He can be contacted at bconnors@eheinc.com.