Scheduling for project success

It is not uncommon to see health care facilities managers directly or indirectly responsible for building projects.
Image by Getty Images
Facilities projects on a health care campus can range from simple office moves to very complex construction and system implementations. Some major construction projects can take years to plan and cost hundreds of millions of dollars to complete. To add complexity to these projects, they often need to be completed while the building continues to see or treat patients.
In the health care field, it is not uncommon to see facilities managers directly or indirectly responsible for building projects. This makes sense given the facilities manager’s broad range of responsibilities as well as their thorough understanding of the multidisciplinary activities within the built environment.
However, what does not make sense is to assume a facility manager has the required training and skills to manage health care construction projects or lead those who manage them. Risk factors are too numerous to count. These projects demand expert leadership to ensure the safety of patients, staff and visitors, and achieve ultimate project success.
Facility project work
Facilities managers in almost all industries are responsible for many different aspects of operations. Whether they work in manufacturing, retail, transportation, production or hospitals, they wear many hats and must know an incredibly diverse range of topics. They must be able to discuss high-pressure steam systems one minute and then provide input on carpet selections the next. They must be able to direct a maintenance crew, understand a financial statement and support countless thousands of square feet of building space.
Much of the work they coordinate could be considered project work. A project, as defined by the Project Management Institute (PMI), is a temporary endeavor undertaken to create a unique product, service or result. These words are very important when it comes to understanding the tools and techniques needed for project success in health care. For example, replacement of an air handler serving a hospital inpatient floor can offer significant challenges for the facilities manager. By PMI’s definition, it would not technically be a project because the result is not unique.
One could argue, however, that the facilities manager would implement project-type planning to replace the air handler without interruption to patient care. It would then be reasonable to see how a facilities manager’s role could evolve to include more and incrementally complex project oversight. As project complexity increases, so do the risks associated with poor performance and unsuccessful projects managed by untrained people.
Defining project success
How does a health care organization define project success? Is it an agreed upon policy statement that is reviewed routinely? Is it just assumed that everyone knows? Time, cost and scope are almost universally identified when the topic of project success is discussed. This is not to say they are not valid components of a good project, but there are factors outside of the “three-legged stool” of time, cost and scope that need to be considered.
What if all three of these criteria are met but the user does not like the product? Imagine a surgeon walking into a brand-new operating room and saying it does not work, even when every scope item was included. If someone is hurt during the project, is it still successful? Consider a project that comes in under budget. If millions of dollars were allocated to a project that were not needed, most likely there were other projects that could not be completed because finances were not available.
The point is that project success can mean different things to different organizations. How project success is measured must be established by the organization before a project starts and may even vary as appropriate. It is critical that a facilities manager responsible for project management understand how success is defined and how accountability will be determined. This information then should cascade as a key message to stakeholders.
Scheduling components
While multiple factors can determine project success, one key element of projects that heath care facilities managers should fully understand is project scheduling. The goal of any project schedule should be to aid the facilities manager and stakeholders in identifying task durations as well as establish overall project duration.
The project schedule is vital in health care and is extremely important for several reasons. First, the schedule is used at a high level to determine the length of the project and determine when operations in the affected area will return to normal. In health care, the schedule indicates when patients can be seen or treated. Second, the schedule is used to identify and plan for interruptions in service utilities such as domestic water, heating, cooling and life safety features.
The facilities manager also can use the project schedule to routinely report on project progress and identify risks to the project based on tasks that appear to be lagging and manage changes as they occur. A schedule of values can be built into a project schedule to assist the facilities manager in identifying actual work performed versus work scheduled. This will ensure that payment is made based on earned value (work completed).
However, a project schedule is only as effective as its inputs. It is not uncommon for the project schedule to be established by the contractor based on input from their trades and subcontractors. This is not to say a schedule prepared by the contractor is inherently inaccurate, but more than likely these schedules are built on pessimistic or worst-case scenarios.
A facilities manager should understand that all schedules are not created equally, and scrutiny with routine monitoring of schedules is necessary as a component of a successful project. Level of detail in project schedule also should be identified in the early stages of project planning.
Scheduling techniques
According to PMI’s Project Management Body of Knowledge Guide (PMBOK® Guide), a project schedule is “the planned dates for performing scheduled activities and the planned dates for meeting scheduled milestones.” The goal of any project schedule should be to aid the facilities/project manager and stakeholders in identifying task durations as well as establishing the overall project duration.
As noted, there are several methods of project scheduling that are available to the facilities manager. There are different scheduling techniques available, such as “program evaluation review technique,” “activity on node” and “schedule network analysis.” Project schedules also can be established simply by ordering activities in sequence to determine project duration.
Critical path schedules shown on Gantt charts or bar charts are arguably the most widely used and recognized scheduling techniques in health care. However, if the facilities manager is not fully fluent in the scheduling technique being used, project success is at risk. Project schedules may be created with the beginning date and end date fixed. The activities of the project can then be inserted to create a timeline.
Project schedules also can be established simply by ordering activities in sequence to determine project duration. This may be done if the project end date is not fixed or the if the project’s start date is flexible.
The key to good project scheduling is providing accurate activity duration estimates. The project scheduler must accurately determine activity lengths so that the project schedule is useful. The schedule baseline provides a means to measure and report project performance by validating value of work completed (earned value).
Critical path methodology
A very common scheduling technique, developed in the 1950s by the Dupont Corp., is the critical path method. In the critical path method, the overall project duration is generally determined by the activity paths with the longest durations, according to the PMBOK Guide. The duration of the critical path usually determines the duration of the entire project.
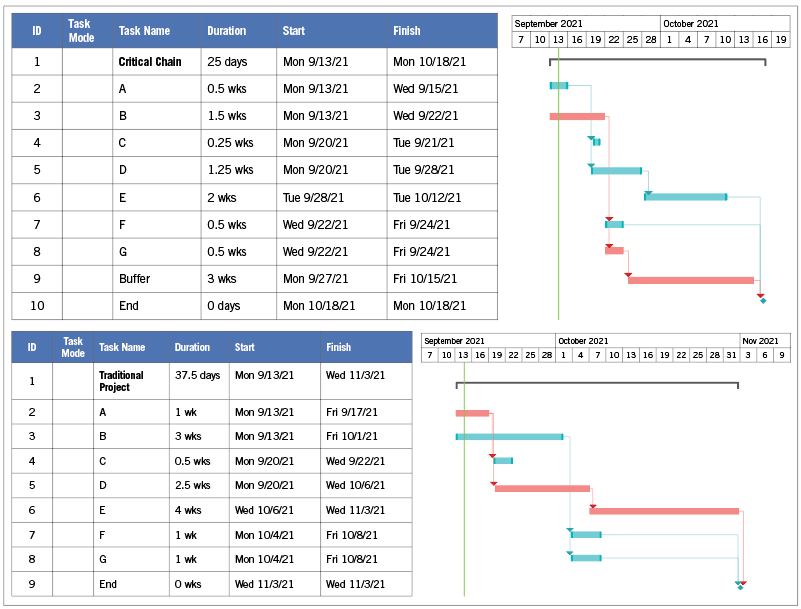
TOP: Critical chain methodology focuses on bottlenecks to improve schedule reliability. BOTTOM: A traditional critical path schedule in Gantt form with critical activities shown in red.
Credit goes here
This technique is useful in determining the amount of flexibility in the schedule on logical task paths. Any delay of a terminal element on the critical path directly impacts the planned project completion date. Also, there is no “float” in a critical path activity, which is the duration a project activity can be delayed without causing project completion to be delayed. Each activity in a critical path schedule is determined by one time estimate.
Frequently, the estimate is pessimistic, which allows for “slack,” or the amount of time a project can be delayed without delaying subsequent tasks. The bottom figure on page 34 is an example of a traditional critical path schedule in Gantt form. Critical activities are shown in red.
The red critical activities and their dependencies constitute the critical path. Again, activity durations are given by one estimate. By estimating the worst-case scenario of each activity, the project has slack or float built in. A good example of this would be installing flooring in a hospital corridor. The facilities manager in charge of the project knows that the task could take as little as three days, should take five days, but could take seven days. Therefore, to ensure the schedule does not slip, the estimate for the task is scheduled for seven days. Any associated activities are scheduled similarly.
One primary problem with critical path scheduling is that time estimates are subjective. Inaccurate activity durations can cause the project to be longer than necessary. Padding task durations is done to ensure a high probability of task completion. The trend is then to waste any padding or slack time at the beginning of the activity. If a problem occurs later, it may be too late to recover. Starting work as early as possible is also common, and this can cause multitasking or jumping from task to task. The result is that tasks then usually take longer and rarely finish early.
There are advantages to critical path scheduling as well. Where the project needs to be accelerated, the critical path helps the facilities manager identify which project steps should accelerate to complete the project within the available time. They are mathematically simple, requiring no complex formulas to determine activity durations. Also, many scheduling software programs support critical path methodology.
Critical chain methodology
An alternative to critical path project scheduling is the concept of critical chain. Research indicates that Eliyahu Goldratt, Ph.D., developed and publicized critical chain, according to the article “A critical look at critical chain project management,” which appeared in the December 2003 issue of Project Management Journal.
Goldratt is also known as the inventor of the theory of constraints, which is the philosophy behind critical chain. The theory of constraints is a tool used in managing repetitive systems based on the principle that every system has a constraint. System performance can only be enhanced by improving or correcting the restraining resource, according to the Project Management Journal article.
Like the theory of constraints, critical chain focuses on bottlenecks to improve schedule reliability. Critical chain recognizes that task durations are not exact. Therefore, task durations in critical chain scheduling have a probability of distribution centered on “most likely” values. Uncertainty is managed by scheduling backwards from when a project is needed to ensure that work that needs to be done is done, and is only done when needed.
A key component of critical chain includes reducing activity duration estimates by 50%. Activity durations are normal estimates, which are typically known to be high probability and contain excessive safety time. The time that is cut from individual tasks is aggregated and inserted as buffers in the project and eliminates resource contentions by leveling the project plan. The critical chain can then be identified as the longest chain of path and resource dependencies (see top figure on page 34).
A project buffer is inserted at the end of the project to aggregate critical chain contingency time. It is then also important to provide resources with activity durations and estimated start times, not milestones. This encourages resources to pass on their work when done.
The project duration in the critical chain figure is the same. However, activity durations have been reduced by 50% to eliminate “safety time” built into each task. Safety time is combined and inserted as a “project buffer.” By using critical chain, the project schedule is only five weeks yet allows for three weeks of buffer. Combined buffer can be less than the sum of individual safety times.
The major advantage of using critical chain scheduling is that it battles Parkinson’s law, or “student syndrome,” which states that work expands to fill the time available for its completion. Even though activities are scheduled to start as early as possible, they rarely do. Another advantage is that the buffers are more realistic, mathematically speaking, than subjective buffers built into critical path schedules. Project times are shortened due to realistic buffering and focus.
There are also drawbacks to critical chain scheduling. For instance, administrators or program managers may be reluctant to approve project schedules that reflect buffers. Their thought may be to remove buffers and shorten overall project duration. Another challenge discussed in the Project Management Journal article is that critical chain only focuses on one of the legs of the three-legged stool: time.
Planning for success
Facilities managers involved in health care projects should understand and develop schedules that are realistic to ensure smooth project performance, mitigate burden on resources and avoid tying up organizational dollars unnecessarily.
Critical path and critical chain scheduling are options available to assist the project team in monitoring project activities and identifying when interventions may be needed. Where time constraints are crucial, critical chain may be a favorable option. Ease of use must also be considered, especially if software is involved.
Schedules are important, and the key to any technique is the accuracy of the data: Garbage in equals garbage out.
Project management in health care
The term “project management” is used loosely in many fields, and health care is no exception. People in any number of formal roles are assigned project management as if it is a skill borne of experience in the field or analogous to other educational or professional backgrounds.
When one reviews any job description for facilities managers, there is a very good chance that “project management” is listed as desired experience, direct responsibility or indirect oversight.
Professional-level project management requires specific skills, tools and techniques so that risk is mitigated and project success is achieved. Patient safety, the ability of staff members to perform their roles at a high level, and stewardship of an organization’s finances demand a very high level of competency from those who manage projects in health care.
Professional membership groups associated with health care facilities management, such as the American Society for Health Care Engineering, do an exceptional service by providing training for job functions that are subject to audit and tailored to meet the requirements of enforceable codes and standards.
Aligning with codes and standards is the interweaving of project management fundamentals that aim to ensure the safety of patients, staff and visitors while project work is being done in occupied settings. For example, documented pre-construction risk assessments (PCRAs) and interim life safety measures (ILSMs) are required in accredited health care facilities.
These assessments and mitigation measures are often, and should be, the work of a multidisciplinary group of subject matter experts in their respective disciplines. However, the needs of the patient demand that these efforts are led by a highly competent facilities manager who has the training and tools needed to ensure project success.
Project management-specific training should be sought or required by those who are responsible for health care projects. It is in the best interest of patients, staff, visitors and organizations.
Gordon Howie, MSPM, CHFM, CHC, is regional director of facilities and construction services at Mayo Clinic Health System in Eau Claire, Wis., and an American Society for Health Care Engineering Advisory Board member. He can be reached at howie.gordon@mayo.edu.




