Nine steps to developing a ventilation management plan

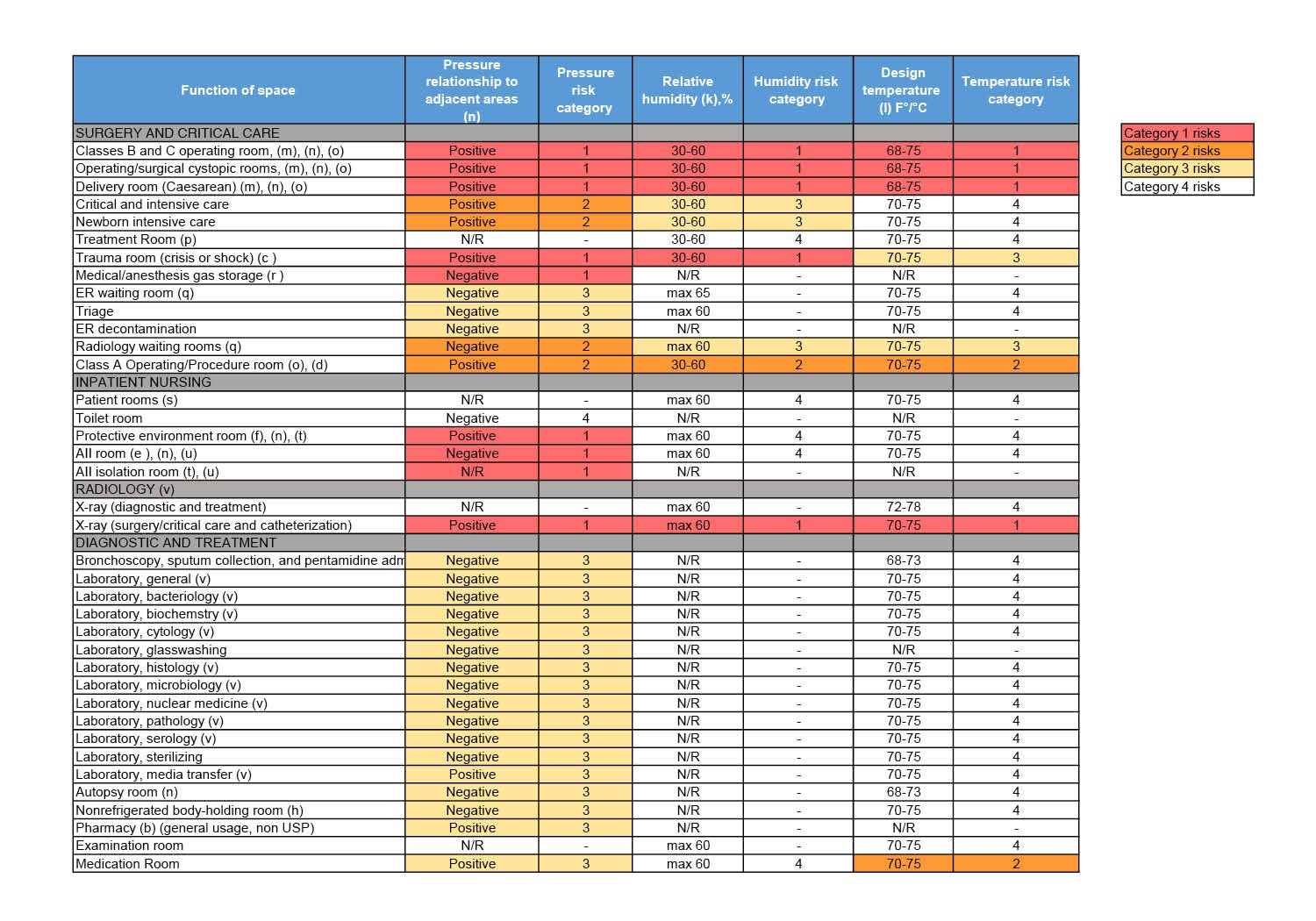
The pressure, temperature and humidity within an OR would likely all be ranked as a Category 1, because the excursion from any of these could be life-threatening during an operating procedure.
Image by Getty Images
Given the increased emphasis on ventilation requirements in health care spaces and the conflicting requirements of various authorities having jurisdiction (AHJs), a comprehensive ventilation management plan (VMP) will help health care organizations manage ventilation and other HVAC systems to maintain compliance with all applicable accreditation, licensure and regulatory standards.
Similar to a water management plan, a ventilation management plan is established and supported by a multidisciplinary committee and aims to identify, develop and implement effective strategies to manage and maintain ventilation and other HVAC systems with a focus on compliance.
Although not yet explicitly required by The Joint Commission (TJC), the Environment of Care Standard EC.01.01.01 requires a utilities management plan, which includes ventilation and other HVAC systems. In addition, a ventilation plan is recommended in an addendum to the 2013 edition of the American National Standards Institute/ASHRAE/American Society for Health Care Engineering Standard 170, Ventilation of Health Care Facilities, and is necessary to ensure that space conditions are within criteria.
Nine-step process
The following nine-step process provides a framework for developing a VMP for health care facilities:
Step 1: Form a committee. A health care facility VMP will need buy-in from a multidisciplinary group of leaders across the organization. Engineering; planning, design and construction; accreditation; infection prevention; nursing; pharmacy; and perioperative services should be represented on the committee. If the organization has multiple sites, it should also include site leaders from each department.
Facilities professionals should consider making the committee a subcommittee of the environment of care (EOC) committee. The ventilation management committee (VMC) can make recommendations to the EOC committee and allows for a direct path to hospital administration.
The VMC may need to meet as often as monthly while the plan is in development. Meeting minutes should be recorded and included with the rest of the documentation for the plan.
Step 2: Determine the code reference. Various codes and standards include ventilation requirements for various spaces, many of which have conflicting instructions. For instance, ASHRAE, the United States Pharmacopeia, the Association for the Advancement of Medical Instrumentation and the American National Standards Institute, as well as state and local codes, all have ventilation requirements. To establish common language and processes related to ventilation and other HVAC requirements, the committee should decide on a single code to enforce in all spaces.
Currently, TJC references the 2012 edition of National Fire Protection Association’s NFPA 99, Health Care Facilities Code, which references the 2008 edition of Standard 170. Table 7.1 within this standard includes design parameters for various spaces in a health care facility.
Typically, organizations adopt the code enforced by their regulatory AHJ with consideration given to adopting more stringent ventilation requirements for specific spaces or areas as defined by the organization. With this approach, there is potential that specific spaces do not meet enforced ventilation requirements due to a conflict in the requirements enforced by the AHJ and the state ventilation requirements under which the space was designed. Each facility should have a clear understanding of spaces in conflict and be prepared to discuss them during a survey.
Step 3: Develop a source of truth. The committee will need to develop a comprehensive list of all the spaces in the facility with ventilation requirements. The facility space management program likely already maintains a list of all spaces in the hospital, so facilities professionals should consider combining efforts. Otherwise, multiple lists will be required to be updated when a space changes use. Facility spaces constantly change to adapt to the needs of the organization. Any change requests should be reviewed by the committee to ensure that the existing ventilation in the space can support the requested change.
This is also a great opportunity to ensure the room usage, room name and the room name on the life safety plans all align. Facilities professionals should take the time to walk each space and confirm that the activities taking place in the rooms match the room name. They also may find that the same types of rooms have different naming conventions, such as “environmental services” and “housekeeping.” Health facilities professionals should consider aligning room names with the code reference the committee chooses to follow.
Step 4: Risk ranking. To prioritize testing and excursion response times, the space element criteria, including pressure, temperature and humidity, should be risk-ranked for each space. Chapter 4 of NFPA 99 outlines four categories of risk: Category 1 are facility systems in which failure of such equipment or system is likely to cause major injury or death of patients or caregivers; Category 2 are facility systems in which failure of such equipment or system is likely to cause minor injury to patients or caregivers; Category 3 are facility systems in which failure of such equipment or system is not likely to cause injury to patients or caregivers but can cause patient discomfort; and Category 4 are facility systems in which failure of such equipment would have no impact on patient care. Applying a risk ranking to each element in the space is an easy, uniform way to rank the criticality to patient care, which then determines the testing frequency (see sidebar above).
Step 5: Excursion response plan. Given the number of spaces within a hospital, it is inevitable that room pressure, temperature or humidity will fall out of range at some point. The risk rankings should be used to prioritize the response times when excursions occur. The committee should determine the required response times for excursions. The results from ventilation testing or monitoring should be documented and presented at the committee meetings. During testing, if there are any deficiencies, the excursion response plan should be followed, and the deficiency should be documented with a work order.
Addendum O to the 2008 edition of Standard 170 allows for temperature set points to be adjusted outside of the range as required for the needs of the patients or at the request of the surgeon. Health care facilities professionals should ensure that these requests are documented and that reports showing temperature or humidity of spaces out of range can be traced back to the request. If automatic reset schedules are not in place, facilities professionals should develop a process to ensure set points outside of range are not left in that state. There are various control strategies that can assist in keeping space ventilation requirements within range.
One strategy is to lock the temperature range within the building automation system to the range decided upon by the committee. This will limit the range of the temperature set point so that users cannot adjust the space temperature out of the set range. Another strategy is having time of day reset schedules to reset space temperature set points to predetermined values at a specific time each day. This will ensure that spaces with set points adjusted outside of the typical range are not forgotten and left in that state.
Additional consideration should be given to this process for critical areas, such as operating rooms, to guarantee patient care is not impacted.
Step 6: Educate the committee. Facilities professionals should dedicate one of the early VMC meetings to educate the clinical leaders on ventilation-related definitions, such as the basic elements of room pressurization, the relationship between temperature and humidity, and the purpose of air changes.
A visual presentation also may help clinical staff better understand ventilation requirements. For instance, facilities professionals can consider creating ventilation maps for pressure, temperature and humidity, and assigning colors to spaces based on the element risk ranking. An example would be red for Category 1, orange for Category 2, yellow for Category 3 and white for Category 4.
For pressure ventilation maps, arrows showing the direction of airflow from each pressurized space will help to depict room pressurization as well as provide clear direction for operational technicians performing testing. For example, each operating room would be color-coded red to show that the pressure ranking is Category 1, but a clean utility room in the same area would be color-coded orange to show that its pressure is ranked Category 2. The doorway to both spaces would have an arrow pointing out to show that the rooms are positive pressure to adjacent spaces.
Another way to educate staff in the hospital is to install an identifier on the outside of each room that has ventilation requirements. This could be a label or a plaque on the room signage, indicating the requirements that apply to the room. It could also be color-coded to match the risk ranking of each requirement. This would make staff in the area aware of the requirements and take ownership over the requirements for their rooms. It would also aid them in speaking about the requirements if questioned by a surveyor.
Step 7: Create a policy. The VMP will need to be defined and published so that it can be referenced by employees in the hospital. It should include the committee members and details, the code references, basic ventilation term definitions, testing frequencies and the excursion response plan. Facilities professionals should consider making it an official policy for the organization. Additionally, existing policies that have ventilation requirements should be reviewed and modified to reference the VMP, rather than indicating requirements in a separate policy.
Step 8: Approval. Each aspect of the plan will need approval from the committee. Once the ventilation plan has been defined, facilities professionals should apply the risk ranking for each element of code-dictated spaces, define the testing frequencies and excursion response process for each risk category, and present them to the committee for approval. They also should provide the list of all spaces with ventilation requirements, room usage type, the assigned risk category and associated testing frequency as well as the excursion response plan. In addition, they should provide the written VMP policy. The committee should review and approve all documents. The approval from the committee should be recorded in committee meeting minutes.
Step 9: Maintain the plan. There are several components of the plan that will require regular maintenance and updates. Facilities professionals should present periodic testing results and highlight any excursions at committee meetings. They also should update the room list as change requests are submitted and approved. As part of routine rounding, each space should be evaluated to ensure that activities in the room or the room signage have not changed. Facilities professionals should stay on top of the code and update the committee as changes occur. Additionally, they should stay current on code adoptions by TJC and evaluate the VMP with each adoption.
Sustaining compliance
A VMP will ensure that critical care areas and noncritical care areas meet the requirements to achieve and sustain compliance as required by TJC’s Environment of Care Standard 02.05.01, Elements of Performance 15 and 16. Additionally, coordination within cross-divisional teams will contribute to more successful regulatory surveys.
The plan also will align cross-divisional efforts to provide a standardized, risk-based review of spaces; their specific ventilation, temperature and humidity requirements; and establish common language and processes related to ventilation and HVAC requirements. Ultimately, a VMP will make the hospital a safer place for patients to heal.
[Editor’s note: A paragraph encouraging readers to adopt newer versions of ANSI/ASHRAE/ASHE Standard 170 was removed from this article. ASHE does not encourage such actions.]
Taylor Vaughn, MBA, CHFM, CLSS-HC, and Brooke Bohme, PE, CHFM, LEED-AP, are facility managers at Children’s Health, Dallas; and Clayton Smith, FACHE, CHFM, is senior director of engineering at Children’s Health. They can be reached at taylor.vaughn@childrens.com, brooke.bohme@childrens.com and clayton.smith@childrens.com.