Identifying and eradicating biofilm
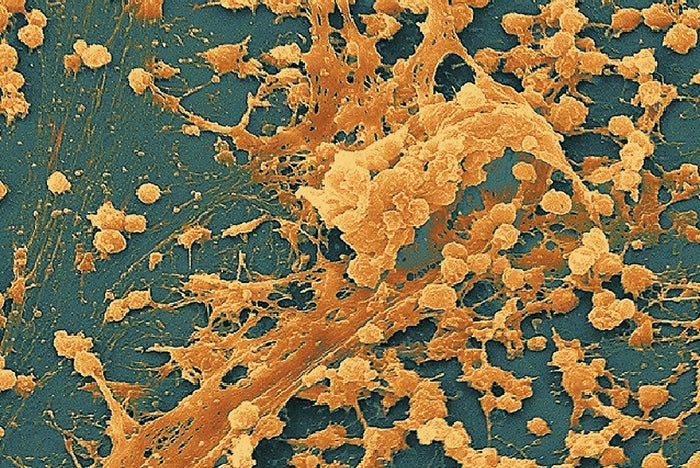
Biofilms serve as protective coatings for microbes to shield them from unfavorable environments.
Photo courtesy of National Institutes of Health
Biofilms are complex colonies of microorganisms that serve as protective coatings for microbes to shield them from unfavorable environments such as heat, ultraviolet light, cold, disinfectant chemicals and antibacterial drugs used in health care.
The components of biofilm greatly heighten bacteria’s resistance to antibiotics, thus enhancing the longevity and potential harm caused by bacteria.
It often appears as slime and discoloring that can be seen in sink and floor drains, buildup around leaking faucets and faucet sprayers, unused toilets and floor mop sinks, hoppers found in soiled utility rooms in hospitals and janitors’ closets in commercial buildings. But biofilm is not always easily seen because it is found in many out-of-the-way locations such as air handlers, air conditioning evaporation trays, water cooling towers, and water coolers, features and fountains.
When biofilm is seen and (most often) not seen, bacteria are present and must be treated and approached with caution and concern.
Biofilm and health
Biofilm has existed as long as bacteria have been on the planet. But it wasn’t until the early 1970s that scientists began to understand the major impact biofilm had on human health; and scientists only began to understand the complexity of biofilms in the 1980s and 1990s.
It is not just an annoyance or another nuisance to be casually addressed by environmental services (ES) or facilities departments. It is an ever-present threat to health and the environment.
Resources
For instance, recent studies and investigations have shown that biofilm has been a major contributing factor in harm caused by improper or incomplete processing of medical devices and implants such as catheters, prosthetic joints and heart valves. Despite standardized processes thought to be effective at sterilizing medical instruments, biofilm is so pervasive and robust that numerous serious patient outcomes have resulted.
Failure to properly reprocess medical instruments to eradicate and remove biofilm during reprocessing of instruments like endoscopes prior to surgical procedures has resulted in infections such as carbapenem-resistant Enterobacteriaceae (CRE) being transferred to patients. As a result, the Centers for Disease Control and Prevention (CDC) established new procedures to ensure biofilm eradication is addressed when endoscopes are processed.
A hospital must be addressed in a universal manner because one area can have an impact upon another — even on other floors or nonintegrated departments. Too often, ES departments are not called upon to address issues found in nonclinical areas of hospitals.
For example, one area not typically addressed by the ES department in its constant pursuit of hygienic patient environments is food service facilities and locations. Biofilm is not only a constant concern as a source of food spoilage, but also food contact and preparation surface contact because, once food contact surfaces become contaminated with biofilm, it is much more difficult to eradicate the exopolysaccharides and bacterial cells of the bacteria.
Eradication and removal
Bacteria communicate and collaborate via chemical interactions for survival. To eradicate and remove bacteria and biofilm from the health care environment, a multidisciplinary and multimodal approach is essential. No one department can succeed and no one department has all the answers.
Biofilm is dangerous to immunocompromised patients. Therefore, removal and eradication must be concentrated and strategically approached.
Multidisciplinary teams must identify potential sites for targeting, which may include hot and cold water supply lines, idle faucets, drains, bathrooms, floors, moist/damp areas, soiled utility rooms, soiled laundry shafts, ice machine drains and dispensing chutes, water fountains, boiler rooms, air vents and many other areas.
Health facilities professionals who are responsible for the hospital environment must recognize that biofilm is not always seen by casual visual inspection and presents a real danger. These disciplines must also recognize that appropriate personal protective equipment (PPE) always should be used when addressing the removal of biofilm as the nature/virulence of a biofilm always must be considered suspect.
Facilities professionals tasked with locating, eradicating and removing biofilm also should be trained and educated regarding why they should look for it, what to look for and how to eradicate and remove biofilm once located.
Often, those responsible for carrying out biofilm removal are just told to “do it” or “get it done” without any specific directions or knowledge. Left to one’s own inventiveness or lack thereof, results are often minimal or even disastrous.
For example, thinking that pouring bleach or a bleach solution down a drain or on a surface will terminate the issue is shortsighted. Biofilm is produced to protect bacteria from harsh environments and disinfectants such as bleach, and antibiotics fall into the definition of a harsh environment.
ES professionals also should recognize that bleach does not clean; rather it is an oxidizer and disinfectant. Hypochlorous acid (HOCl) is an Environmental Protection Agency (EPA)-registered, hospital-grade disinfectant that is as effective as bleach (if not more) in the biofilm-abolition process and is much safer for the environment, metals, staff and PPE. The odor is not noxious and thus safer for all concerned, particularly if removing biofilm from a closed and fresh-air-deprived environment.
Additionally, hospitals are subject to EPA regulations regarding discharge of residual chlorine into wastewater. If an incorrect solution is applied, the possibility exists of exceeding the maximum residual chlorine level into the waste stream.
HOCl is considered a safe alternative to bleach for its disinfecting ability and is safer for personnel to use. However, ES professionals must have a complete understanding of both bleach and HOCl reactivity. With both solutions, there is still the potential for danger if ammonia is present. Both solutions, when mixed with ammonia, are hazardous. Neither HOCl nor sodium hypochlorite should ever be introduced directly into any drain without first flushing the drain with clean water. If ammonia in any form is present, doing so may result in chloramine gas being released, which may cause respiratory distress or death.
Disruption and eradication
Biofilm in the health care environment — as opposed to being present on implants or other implements introduced into a body — must be disrupted through mechanical or physical action.
Once a multidisciplinary and multimodal team has been identified and trained, how the process is implemented is vital. The following actions may be used or adapted by ES professionals:
- If possible, determine the type or identity of the biofilm to be removed to know the best process to implement.
- Discuss what chemical/disinfectant is to be used and how it is to be applied.
- The decision to manually scrub with a brush and a bucket of cleaner/disinfectant is usually one of the first to be considered and dismissed. But, just as in medicine, the guiding principle for removal and eradication of biofilm should be to use the most appropriate and efficient method without disrupting or causing harm to surrounding areas.
- Scrubbing or high-pressure spraying is most often the choice, but must be appropriate to the environment and conditions personnel may encounter. Methods and chemicals will be dictated by accessibility, electrical considerations, the patient care environment and restricted areas such as pharmacies, intensive care units or research labs.
- Steam is also one of the most useful multimodal interventions that can be used in combating biofilm. Two types of steam generators are normally available for health care ES: low-pressure/high temperature electric powered, usually with a self-contained steam chamber that uses manual effort in combination with mechanical action (brushes or microfiber cloths) designed for small spaces; and high-pressure/high-temperature generators that are fully electric or a combination of electric/gas units connected to water supply sources via hoses. These units rely on high-pressure water nozzles to disrupt and remove biofilm. The high temperature of both types of generators dislocates and kills the cells, and the manual or mechanical pressure physically removes the biofilm and most biofilm molecules from surfaces. Again, the environment in which the biofilm is located must be considered.
- The physical removal of the biofilm must be followed by removing any remaining contaminated water from floor, metal or other surfaces lest any bacteria remaining be allowed to repopulate the contact surfaces.
- The previous step should be followed by a clean-water rinse followed by an application of a properly diluted solution of a germicidal agent such as HOCl.
Proper and appropriate PPE must be used and documented. Implementation of the buddy system — especially in closed and potentially dangerous environments — must be followed.
ES professionals must use safe and effective cleaners and disinfectants for cleaning and disinfecting brushes, wipers, buckets, scrapers, mops, steam generators, wet vacuum cleaners and attachments, and clothing/footwear that may have been contaminated. Proper hand washing after completion of the assigned tasks must be followed as well.
Training required
Proper processing of clinical and aesthetic surfaces (cleaning and disinfecting with proper tools that trap and remove bacteria and unseen biofilm) is an essential step toward the goal of a healthy, hygienic patient care environment. Biofilm will never be completely eradicated from the health care environment, but every reasonable effort to prevent its presence and proliferation must be taken.
Formal training of ES and facilities staff regarding the virulence and ubiquitous nature of biofilm must be a priority.
The Association for the Healthcare Environment’s Certified Healthcare Environmental Services Professional, Certified Healthcare Environmental Services Technician and Certified Surgical Cleaning Technician programs are excellent first steps in addressing the importance of proper processes and techniques to address biofilm.
John Scherberger, FAHE, CHESP, is president and founder of Healthcare Risk Mitigation, Spartanburg, S.C. He can be contacted via email at jfscherberger@me.com.