Study addresses barriers to using UV disinfection
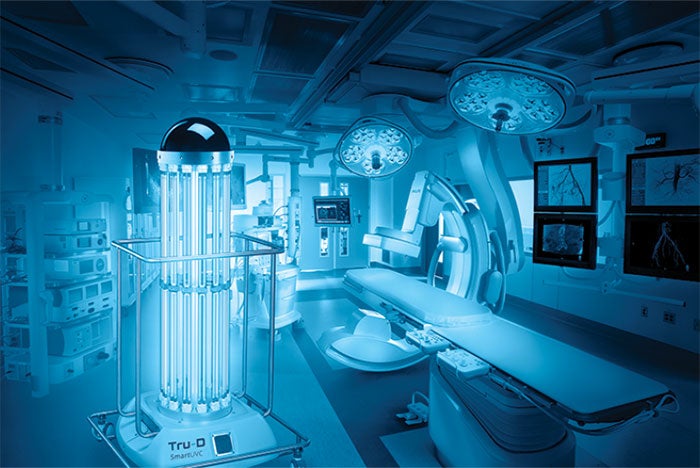
Tru-D disinfecting an operating room
Tru-D SmartUVC
In the Benefits of Enhanced Terminal Room (BETR) Disinfection study, researchers from Duke University set out to prove what many concerned with infection prevention have long suspected: Using ultraviolet disinfection systems helps to reduce health care-associated infections.
However, because a tool is only as good as its user, the researchers have published a follow-up study that addresses the most frequent barriers hospitals faced in implementing UV systems and strategies to overcome them.
The study identifies two key barriers: timely and accurate identification of rooms that would benefit from UV disinfection, and overcoming real or perceived time constraints to allow environmental services (ES) staff time to properly use the system. The researchers then defined five implementation strategies used during the two-year study that involved nine southeastern U.S. hospitals.
The first is to establish UV disinfection as a patient- and staff-safety priority. The study’s authors report that doing so helps to overcome conflicts in opinions among nurses, bed control personnel and ES. Next, hospitals must establish regular communication. During the study, ES, nurses and bed control personnel had daily, direct communication that helped to facilitate bed assignment and schedule rooms that needed enhanced cleaning. Other strategies include:
• Deploy the UV device even if the cycle time needs to be cut short because a patient is being admitted.
• Track compliance and share the data with staff.
• Gather necessary resources, such as ensuring enough staff during peak times.
“These UV machines don’t do any good unless they are actually used,” explains Deverick Anderson, M.D., MPH, FSHEA, FIDSA, director of the Duke Center for Antimicrobial Stewardship and Infection Prevention. “We hope hospitals can use the lessons learned.”


