Supporting the four methods of simulated training
Medical simulation centers can be designed to enable people to practice medicine safely in a number of ways. Joseph O. Lopreiato, M.D., MPH, CHSE, president-elect of the Society for Simulation in Healthcare (SSH), explains that a comprehensive simulation center utilizes four methods of simulated training.
The first is a standardized or simulated patient (SP). An SP is a person portraying an individual in a health care situation, such as a patient with a particular medical condition, someone in the midst of a mass casualty event or an agitated family member. (A Healthcare Simulation Dictionary is available for download on the SSH website at www.ssih.org/dictionary.) These types of simulations help to assess how well a learner interacts with people while doing things like communicating medical information, taking a medical history or performing a physical exam, says Lopreiato.
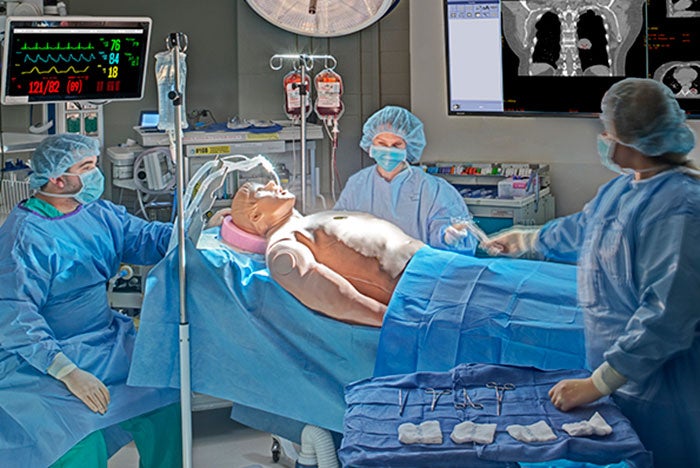
Mannequin-based simulation involves the use of full-body representations of human beings. These simulators demonstrate varying degrees of physiologic function and fidelity and are particularly useful for practicing trauma or emergency situations. Highly sophisticated mannequins have realistic skin and hair, can react appropriately to different medical gases and are capable of producing lifelike heart and lung sounds, pulses, movement (such as seizures or eye blinking), blood and other fluids, and vocal interaction.
Task trainers represent just part of a human body, such as the chest or head. These devices are used to train people in the key elements of a task or skill like central line insertion.
Finally, virtual and augmented reality technologies are used to practice techniques like cardiac catheterization or laparoscopic surgery.
A full-service simulation center is designed to support each of these training methods, says Lopreiato. “It shouldn’t be a one-trick pony. You want to be able to use the approach that’s best-suited to accomplish your learning goals and objectives,” he says.
These techniques can be used to train individual health care professionals, whole medical teams or home caregivers. When medical errors occur, the error conditions can be re-created in a simulated environment in an effort to recognize safety issues and prevent a recurrence. Simulated care environments also can be used to test facility designs and identify latent safety threats. For a hospital undergoing renovation or building a new patient wing, “simulation can be used to practice care in the new spaces,” says Lopreiato. This way, any defects in the design can be corrected before it is built out.
Amy Eagle is a freelance journalist based in Homewood, Ill., who specializes in health care-related topics She is a regular contributor to Health Facilities Management.