How integrated facility design can transform health care facilities
Health care reform and financial challenges are causing health care systems to reconsider how they invest capital for facility infrastructure. The foundation of integrated facility design (IFD), or what some organizations have identified as Lean design, is on the forefront of leveraging Lean principles to deliver breakthrough results in the design process and make the most of one of the large capital investments. IFD systematically applies Lean principles and concurrently integrates the expertise of all stakeholders — patients and families, hospital administrators, physicians and surgeons, nurses, staff, the architect, the general contractor and Lean experts — to achieve breakthrough improvements when compared with traditional design.
Lean transformation and IFD provide dramatic results in removing waste from current health care building projects. Lean innovation is defined as the creation of services for the future, with a rapid and disruptive continuum shift in performance and cost that separates itself drastically from the industry performance standard. As the face of health care is being reshaped, so should our thinking about the design process. Sustainable, repeatable methodologies and approaches to IFD coupled with the current Lean transformation efforts and infrastructure being built within health care organizations will deliver measurable improvements in engagement, quality and safety, service, cost and growth.
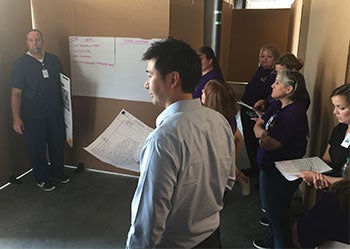 |
| Testing design concepts can narrow alternatives and help to decide the best options. |
Integrated facility design uses concurrent engineering methodology during the design process to accelerate idea generation. That is where multiple sets of design assumptions are tested to eliminate alternatives. This method provides the design teams with opportunities to overlap multiple scenarios and reduce the cycle time of an individual set, thus reducing the lead time of the design process. Compare this to point base design where only one design assumption is tested throughout the life cycle, resulting in a longer process.
During the IFD process, the expert applies Lean principles in the following ways:
Workflow analysis. This allows the design team to see where their layout adds value and where it creates bottlenecks and waste. IFD will challenge individuals to think about the system at a macro level to eliminate waste. Specifically:
- Care coordination and delivery are major issues at many organizations around the country. By analyzing time required to deliver care, known as cycle time, and “takt time”, which evaluates demand vs. cycle time, IFD helps health care companies to determine the optimal number of rooms and beds, reducing costly square footage compared with typical design estimates.
- 5S (workplace organization) and “activity follows” determine the optimal layout of furniture, equipment, and supplies in rooms and work spaces.
- Standardized work planning establishes optimal work sequences and timing so providers, nurses and staff can make the most efficient use of the new layout.
- 7-Way Scenario scorecard tracks improvements achieved to help the integrated design team see opportunities for future layout changes. Design teams track improvements made in the design relative to the initial baseline layout.
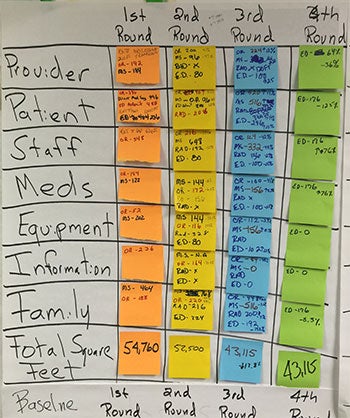 |
| Listing the objectives of each department will inform decisions during the design process. |
Linking design metrics to “True North” metrics. IFD first links the design metrics to the organization’s “True North” metrics, which are the governing objectives of an organization. It considers the objectives related to physician and staff engagement, employee safety, quality, cost, patient experience and growth. Once understood by the design team, the metrics keep them focused on the organization’s strategic plan before moving forward. Throughout the process, the integrated design teams use IFD guiding principles to align all stakeholders to Lean principles and guide the decision-making process. Guiding principles include:
- Start with the customer.
- Too much space is an enemy.
- Base the design on flow optimization, not department optimization.
- Use load leveling to reduce space requirements.
- Reduce lead times to decrease space requirements.
Evaluating organization values. The IFD process moves your organization's values, beliefs and principles down to chairs, drawers and lights through five phases:
- Project management and governance
- Conceptual design at the systems level
- Functional design at the value-stream level
- Detailed design at the operational level
- Standard work development for operating in the new design
Keeping patient value at the forefront. IFD includes representatives from the core services: internal medicine, physicians, lab, radiology and pharmacy in the planning and implementation. The process also includes facilities personnel, as well as patients and architects. All team members should be included and can add value to the process, thus adding value to the patients. When working with providers in a clinical or hospital setting, it is important for them to be comfortable with how the data are gathered, understood and reviewed. IFD, like Lean transformations, is a new concept to many providers. The IFD approach guides the area leadership and clinical staff to understand the process and data, and to reach agreement on what the data represent. This buy-in of the process and data is crucial for teams to successfully move forward.
The IFD approach in working with patients, physicians, design teams, management, staff and partners has made an indelible impact. Innovations in the creation of patient value expand the scope from the core clinical processes to consider a wide array of issues, including patient preferences, technological possibilities, financial arrangements and integrated patient journeys. Large health care organizations around the world are taking advantage of the benefits IFD offers.
Case 1. Northeast Georgia Physicians Group uses IFD to culminate patient experience
Northeast Georgia Physicians Group (NGPG) began its Lean journey several years ago. Historically, NPGP designed its clinics using a traditional one-size-fits-all approach. In designing the new clinics for OB/GYN and urology, NGPG chose a nontraditional approach and used IFD and Lean principles. “This provided us with the much-needed structure to incorporate Lean within the design of our clinics,” says Tina Walden, executive director. “We engaged all members of the health care team as well as our patients. The top priority was to design our clinics to support the ideal workflow in order to provide the highest level of value to our patients. It was important to design the space to be flexible and adaptable. Our design is finished, and now the real work begins. It was amazing to watch the transformation of the team through this process. We are confident that the clinics have been designed to promote the ideal patient experience.”
Case 2. Health care organization becomes showcase for IFD
IFD recently supported the leading hospital in a major U.S. city, which is chronicled in the book Leading the Lean Healthcare Journey. By utilizing Lean and IFD principles, this hospital was able to achieve significant results at its ambulatory clinic located off-site from the main campus. The integrated team reduced construction costs by $25 million, reduced total square footage by 28 percent, and improved the patient and clinical staff experience by double-digit numbers. Health care organizations from around the world visit this facility yearly to study the hospital’s use of IFD principles and learn how it also deployed the Lean Management System to support its design assumptions.
Case 3. Large health care network saves more than $1 million in reduced space requirements
IFD also was successfully implemented at one of the largest independent multispecialty groups in the country. In renovating its entire facility over one weekend, this client showcased that providing a time-based schedule and ability to solve and adjust is one of the most critical outputs of effective use of IFD.
In general, IFD has been shown to reduce the number of change orders during the building process that can sometimes add up to 20 percent or more additional costs in traditional project management. Here are some specific improvements made at health facilities that used the IFD approach:
- Standardizing rooms can result in less patient waiting and less wasted provider care time. By knowing how many of each item should be in the exam room every day, organizations can centralize inventory, restocking and ordering medical supplies through a facilities department.
- A health clinic had plans drawn for a new location. Its original plan called for 43,000 square feet. Through the IFD design process the need was determined to be 38,000 square feet, a greater than $1 million cost avoidance. This also allowed for the addition of imaging and visual services, which were revenue enhancements for the practice at no additional square footage.
- One facility improved patient flow and reduced its average cycle time for a patient visit by greater than 20 percent, freeing up time for other deferrable tasks such as prescription refills and calls to patients on results. Other improvements noted by patients are easier navigation and improved communication. Patient satisfaction scores have improved at a double-digit rate measured by the likelihood with which patients would recommend the practice.
- Another facility reduced the space needed for emergency department (ED) and operating room (OR) equipment from the initial program of a critical care tower. This allowed the departments to achieve lead-time reductions during future-state mapping. The ED and OR teams continued to achieve patient movement reductions through schematic events and made significant reductions.
As health care organizations continue looking for strategies that eliminate unnecessary costs, design and construction methods that bring projects in under budget should be one of the channels they keep their eyes on.
Doug Dulin is a global practice leader of integrated facility design for Simpler Consulting, Raleigh-Durham, N.C.




