Weigh human factors, systems engineering in infection prevention
 |
Hospitals that hope to achieve significant reductions in complex health care-associated infections like Clostridium difficile should carefully analyze their entire work systems and human-factors engineering in addition to reviewing isolated practices of health care workers.
That’s one key finding from a multifaceted study published in the March issue of the American Journal of Infection Control. The study, conducted between September and November 2013 at a large academic medical center and an affiliated Veterans Administration hospital, assessed compliance of health care workers and visitors with all areas requiring contact isolation precautions.
The study’s authors noted that such traditional infection prevention interventions as improving physician or nurse hand-hygiene compliance will be “inadequate” to address complex health care-associated infections such as C. difficile.
Researchers used direct observations to collect data on the current practices of health care workers who care for patients with C. difficile. They also measured the time required to complete contact isolation precautions and assessed the adequacy of contact isolation supplies.
Data from the study were based on 288 direct observations of nurses, physicians, visitors, environmental services staff and other types of health care workers at the two facilities. Among the highlights of the results:
• Full compliance with established contact isolation precautions was low at both hospitals. At Hospital A, 7 percent (or 17 people observed) complied with all contact isolation precautions, while at Hospital B, the full compliance rate was 22 percent (based on 11 persons observed). Full compliance was defined as using alcohol-based hand sanitizer or hand washing with soap and water; donning of gown and gloves; room entry; room exit; removal of gown and gloves; and hand washing with soap and water.
• Full compliance with contact isolation precautions compared with noncompliance required a significantly greater amount of time before room entry, inside the room and after exiting the room.
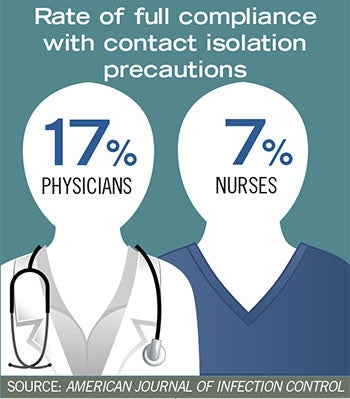
• Interestingly, physicians had a significantly higher rate of full compliance compared with nursing staff (17 percent vs. 7 percent).
• Hand hygiene prior to glove use was the most commonly missed component of contact isolation precautions.
In evaluating work systems and human factors, the researchers noted that patient room layouts need to be considered when analyzing issues affecting compliance with such precautions as hand washing.
“The presence of multiple sinks inside patient rooms may increase the rate of appropriate hand hygiene (i.e., soap and water) on room exit, especially in the academic setting with large medical teams of residents and students,” the authors explained.
Study data also showed that no visitors observed were fully compliant with contact isolation precautions. “Although visitors are less likely to visit multiple patient rooms as [health care workers] would,” the authors stated, “they may represent a vector for nosocomial spread of C. difficile into common areas.” They also noted that neither hospital in the study had a consistently implemented infection prevention policy addressing visitors of patients under contact isolation precautions, and that this represents “a gap in CDI [C. difficile infection] prevention.”


