Flexible facilities
About this articleThis feature is one of a series of quarterly articles published by Health Facilities Management in partnership with the American College of Healthcare Architects. |
Health care facilities are highly complex and function-specific structures that must respond to multiple conflicting demands over their lifetimes. At the same time, the nation’s health care systems have a high level of future unpredictability.
Hospital buildings, therefore, face an indeterminate future in which they must function with a high degree of accuracy yet remain viable for a period of time even as technology changes.
One thing is clear: It will take new thinking about health care, health care buildings and their design to move forward. Now, more than ever, lowest life-cycle costs and continuous performance at optimal levels will be critical for long-term success.
Adapting to change
Buildings need the flexibility to change and adapt to new needs and conditions. Health care architects have been good at working around the edges of this issue through a series of techniques to address flexibility or adaptability in buildings. They include:
One-hundred-year site. This considers the very long-term outlook for the community, access, utilities and other elements from the beginning of site selection.
Empty chair. This leaves an area on the campus to start incremental replacement of obsolete buildings.
Armatures. This plans major corridors to be permanent and allows growth and change around them.
Multiuse spaces. This plans space and building configurations for flexible uses over time.
Modular planning. This organizes multiuse space in clinics and other areas with repetitive designs.
Scenario planning. This anticipates alternative futures and plans the ability to accommodate them all, if possible.
Soft space. This plans for space that can be relocated to allow expansion of high-tech spaces.
Template plans. This is used to build on multiple sites in a short period of time.
Interstitial space. This is used selectively over high-tech spaces.
Modular utility systems. This is for selective shutdown of mechanical and electrical systems when not in use or when under repair.
These and similar ideas are excellent strategies for enhancing the ability to accommodate change, but they are not enough.
 |
| IBS was used creatively to achieve flexibility at Michael E. DeBakey VA Medical Center in Houston. Photo courtesy of SmithGroupJJR |
Hospital study findings
In an unpublished survey sponsored by the Department of Veterans Affairs (VA) in the early 1970s, 10 hospitals in the private sector and 10 within the VA system were studied in detail to document changes and costs of change.
In one facility, as much as five miles of telephone wire was installed during the first three years of occupancy (this was before computers). In another example, an older hospital had moved its central supply department five times. The survey provided clear evidence that the main inhibitors to change and contributors to the disruption of patient care, downtime and cost were the mechanical-electrical-plumbing (MEP) systems.
Any building planned to accommodate change needs to have adaptable MEP and structural systems. Many designs do not accomplish this adequately. In the VA survey, for instance, approximately five times the original construction cost (not counting inflation) was spent on major renovations of an acute care facility over a typical lifespan of 50 years. In today’s high-tech environment, one can assume that the rate of change has increased substantially.
The VA research study went on to develop a proposal for strategic integration of MEP and structural systems using modules that could be reorganized to accommodate almost any architectural design [see sidebar, Page 40]. The VA calls it the VA Hospital Building System and recommends its use for major VA hospitals. In the private sector, it is better known as an Integrated Building System (IBS). The details of the IBS periodically have been updated and may need to be brought up-to-date again to reflect technological and operational changes.
The IBS can be thought of as a set of rules and a kit of parts, with the rules being the most important. Project team members should:
Identify permanent vs. adaptable elements. This requires identifying building elements that cannot be economically changed versus those that can be changed easily without excessive cost or disruption. Elements considered permanent should be designed for a probable range of uses rather than for a specific first use. For example, air trunk ducts might be oversized so they will not have to be ripped out if the air supply needs to be increased in the future.
Utilize modular planning. The building should be planned as a series of modules, each with the same organizing principles. Each module’s utilities mostly will be independent of others. This way, one module can be shut down to upgrade services without affecting other parts of the building. Some modules can function on a 24-hour-a-day schedule and some on a reduced schedule to save energy. The modules do not need to relate to the functional planning.
Minimize structural constraints. One example of this is providing a long-span structure in at least one dimension to allow sufficient flexibility in functional plan layout and to accommodate any future changes without interference from columns or shear walls. When the study was developed, 40 feet was considered a minimal structural span. Floor loading also should be designed to accommodate a reasonable range of functions in each building module. The functions and resulting floor-loading criteria may vary in different areas of the building.
Organize utility operations. This includes organizing vertical and horizontal zoning for all utilities so that each utility has a defined zone in both directions. Zones also should be provided for services that are not needed initially but might be required later. For example, include a zone for a return air duct where initially there is only a need for an exhaust system.
Separate function from utilities. Clinical and other functions should be separated from utility distribution with a walk-deck ceiling system. This way, tradespeople can work above and below the walk deck simultaneously, compressing the overall construction time. Subsequently, utilities can be changed or upgraded above the walk deck as functional needs change, with minimal disruption to patient care or other essential activities.
Plan for service bays. Vertical risers in each module should be reduced or eliminated. They can be clustered at the perimeter of the module in a service bay. This way, it is possible to change the functional plan layout without having to accommodate plumbing stacks that pass through to other floors.
Adapt the construction process. IBS construction allows significant savings in labor and fieldwork by maximizing repetitive modules and speed of construction. Training of cost estimators and potential construction general contractors and subcontractors must be included to take advantage of these savings.
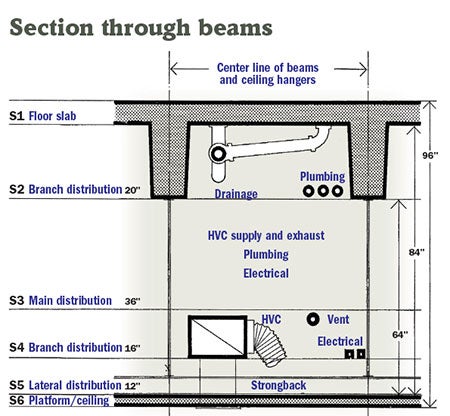 |
| A sectionalized drawing of the service zone above the walk deck illustrates the vertical organization of the system outlined in the VA research. Source: VA Hospital Building System — Application of the Principles of Systems Integration to the Design of VA Hospital Facilities, 1977 |
Implementing the results
At the end of four years’ research, development and acceptance, the team comprising two health care design firms (Stone, Marraccini and Patterson; and Building Systems Development) and two technical consultants (Rutherford + Chekene; and Ayres, Cohen & Hayakawa) was awarded a design contract to implement the research findings with a 500-bed demonstration project at VA Loma Linda Healthcare System in Southern California.
It was completed more than six months sooner than a conventional project with substantial reductions in the cost of some building components, including mechanical systems and interior partitions. However, there were offsetting additional costs for the exterior skin and the walk deck.
Construction cost was within the prevailing norm at the time and change orders were reduced to almost none. In fact, the contractor had nothing but praise for IBS. Significant savings accrued to the contractor and the subcontractors that were not recognized in the bidding process and, therefore, were not passed on to the owner due to the experimental nature of the project. Operationally, the amount of patient and workflow disruption was reduced substantially and the ability to accommodate change was enhanced greatly.
Maintenance costs were less than the prevailing norm, subsequent remodeling costs were reduced substantially and the ability to change space as needed was enhanced. Moreover, sustainability was increased because the building’s ability to adapt has extended its useful lifespan.
The project now has been in operation for more than 30 years and, during that time, has been changed frequently and continues to perform well. In fact, an estimated 30 percent cost reduction reportedly was achieved in the IBS building during renovations where the MEP systems were involved. These savings do not include the cost of downtime and loss of functionality during renovations, which also can be considerable.
The cost reductions come from several sources. For example, if there is a need for a new 220-volt outlet in a patient room, there is a zone above the walk deck for electrical distribution. Moreover, power sources have been designed for a range of uses so adequate power likely will be available. Access to the correct circuit can be obtained easily above the walk deck and the wires in a conduit can be dropped down in the wall into the patient room. Finally, only a small opening need be made in the patient room wall for a back box and plug that can be installed quickly.
Using this example in a conventional building, a circuit would have to run from a panel box through the corridor’s existing ceiling space and any connections would need to be made in the corridor on a ladder and then fished into the patient room where the ceiling and wall would be disrupted.
It is easy to imagine this example played out in an IBS building at a larger scale when changing out radiology or surgical equipment, converting from recirculate to total exhaust air systems or expanding an existing emergency department while maintaining day-to-day operations.
Challenges of IBS
So, if IBS is so good, why has it not been used more in the private sector? Largely because IBS design, construction and operations require a new way of approaching design and construction by the entire team.
For one thing, the owner must be on board and supportive of a somewhat experimental design and construction process. The design of the architecture, MEP systems and structure also must be accomplished simultaneously in an interactive environment as opposed to designing first and stuffing the MEP systems in afterward. Additionally, designing each component for its lowest cost will not work — lowest system cost is the goal.
Modest additional fees also must be considered for the design team to allow for the learning curve and a higher level of documentation. Building information modeling will enhance this process. Rigid redesign requirements will make the team wary of taking on something new, so these expectations may need to be modified depending on the team’s past experience.
Conventional cost-estimating methods based on quantity takeoffs will provide an inflated cost estimate. Study of previous IBS projects and construction methods is required to obtain accurate estimates. The contractor and subcontractors must be educated prior to bidding on these buildings about how to save time and money in their construction. Fortunately, there are enough examples of facilities around the country to visit and learn from.
There may be some additional first construction costs, but these can be minimized. In studies by the VA, the cost of the many completed IBS buildings generally falls within the 75 percent median of the Reed Construction Data Inc.’s RSMeans cost data for hospitals. The demonstration project in Southern California did not cost any more than a conventional VA hospital. However, that was a period of high inflation and the savings in construction time offset any increased cost of materials.
In some cases, when adding to existing conventional buildings, the greater floor-to-floor height of IBS imposes constraints that make this approach impractical. For others, a system of gentle ramps or skipping some floor connections will work to establish a new level of floor-to-floor heights for the hospital’s addition and other additions and replacements in the future.
A changing world
The Affordable Care Act is generating new health care building types, not all of which are suitable for IBS projects or the longevity they provide.
For acute care facilities, however, lowest first cost should not be the main motivation for design decisions. In fact, any such facility should be planned to last for 50 years or more.
An IBS approach will not solve all the problems of premature obsolescence, but it will go a long way toward extending the building lifespan and lowering the costs of renovation as time passes.
Accessing the original VA research
Released in 1972 and revised in 1977, the VA Hospital Building System — Application of the Principles of Systems Integration to the Design of VA Hospital Facilities research study report (www.wbdg.org/ccb/VA/VASTUDIES/hospital_bldg_system.pdf) consists of three parts: a design manual, a database and a project report.
The 800-page document provides an in-depth look at the Department of Veterans Affairs-sponsored research leading to a proposal for strategic integration of mechanical-electrical-plumbing and structural systems using modules that could be reorganized to accommodate almost any architectural design.
In 2006, a 122-page Supplement to VA Hospital Building System Research Study Report (www.wbdg.org/ccb/VA/VASTUDIES/hospital_bldg_system_supp.pdf) was released to address the effects that 30 years of changes in technology, construction practices and health care models had on the original report findings.





