Despite progress, more work needed on infections
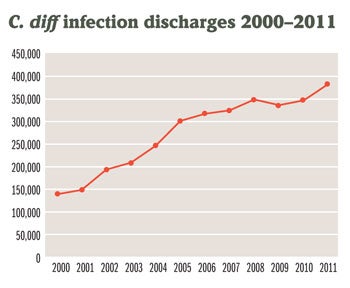 |
| The graph shows the increase in the number of patients with community-onset or HAI cases of Clostridium difficile from 2000 through 2011. Source: Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project |
The Centers for Disease Control and Prevention (CDC) reports that while progress is being made to prevent health care-associated infections (HAIs), continued gains will require vigilance by clinical and environmental services (ES) staff.
The CDC's recent "National and State Healthcare Associated Infections Progress Report" shows that reductions were reported for nearly all infections between 2011 and 2012, including two particularly impacted by hand hygiene and environmental cleaning.
Reductions include a 4 percent drop in hospital-onset methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections and a 2 percent decrease in hospital-onset Clostridium difficile infections between 2011 and 2012.
Overall health care-associated invasive MRSA has decreased 31 percent since 2008, based on surveillance that predates the HAI progress report, CDC states.
The decrease in C. difficile infections, however, fell far short of the 25 percent reduction that was targeted for the 2013 reporting year.
The report helps to measure progress toward the five-year HAI prevention goals outlined in the "National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination" set in 2009 by Health & Human Services.
"We have more we need to do with C. difficile, it's at historic highs," says Cliff McDonald, M.D., medical epidemiologist, division of health care quality promotion, CDC.
McDonald says there is good news associated even with the small decrease. "The fact that C. difficile is plateauing and not going up is a good thing, but it certainly needs more work."
More work means continued focus on the critical role of ES and hand hygiene, which build on one another to reduce infections, he says.
"We are trying to refocus people to understand that ES is an integral part of patient safety. For a long time, ES staff were seen as a part of the hospital that was important for aesthetics and getting better patient satisfaction scores, but it's more than that.
"It's about maintaining an environment that's safer and reducing the bioburden that's on a variety of patient room surfaces. That's especially true with C. difficile because it's a spore that persists in the environment so easily," he says.
Hand hygiene is the critical last line of defense against the spread of MRSA, C. difficile and other bacteria, he notes. "If you can get someone to clean his or her hands each time before he or she touches a patient or goes into a patient room, then you're preventing that transmission."
McDonald says the ultimate goal is to eliminate HAIs but, in the interim, the focus is on driving down the number of cases using existing technologies while assessing the efficacy of new technologies and methods.
The CDC is studying the effectiveness of ultraviolet light irradiation, which some hospitals are using for patient room disinfection.


