Extra Efficiency
 During these tough times, hospital planning and design professionals must stretch capital dollars while responding to capital improvement needs. One approach is to examine principles of "lean" design, or Kaizen, to determine what lessons can be used to advance hospital processes and functionality without spending a lot of money.
During these tough times, hospital planning and design professionals must stretch capital dollars while responding to capital improvement needs. One approach is to examine principles of "lean" design, or Kaizen, to determine what lessons can be used to advance hospital processes and functionality without spending a lot of money.
Kaizen is the Japanese word for improvement and refers to a philosophy or group of practices focusing on continuous improvement in manufacturing, business activities and even life. It focuses on seven types of inefficiencies that should be minimized or eliminated, including transportation, inventory, motion, waiting, overproduction, overprocessing and defects.
While it is easy to imagine how these inefficiencies might impact the manufacture of a complex product such as a magnetic resonance imaging machine, it may seem like a stretch to apply these principles to a hospital. However, most health care planners and designers include on-site observation in their toolkit of pre-design and programming processes. The data gathered in on-site observation often result in planning changes to reduce staff steps and increase effective use of both patient spaces and support areas.
Designing out inefficiencies
Many concepts developed to reinforce these planning goals are examples of lean design and address the seven types of inefficiencies. Each example is designed to improve hospital functionality and processes without large capital expenditures.
Transportation. This requires improving hospital efficiency by reducing the travel of materials, equipment and people.
By keeping materials close to the bedside, staff can reduce travel from central supply areas for patient care. This might be implemented by utilizing locking procedure or supply carts at the patient's bedside. Nurse-server millwork also can be installed outside patient room entrances, adjacent to decentralized nursing stations or alcoves.
Something as simple as adding bedpan washers to inpatient toilets can reduce staff travel greatly, allowing the staff to remain in the room instead of carrying bedpans to the utility room.
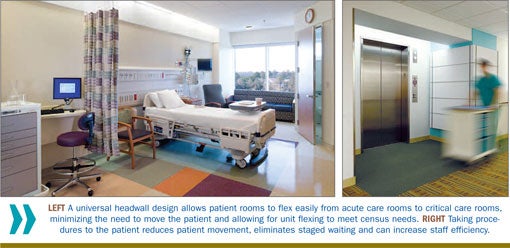
By designing the patient room as a universal room, with a headwall hefty enough to support critical care, patients can remain in the same room regardless of their acuity, thus eliminating transport. In addition, taking diagnostic procedures to the patient instead of having the patient go to different departments reduces patient transport.
Health care providers must determine which procedures the hospital can transition easily to this type of care delivery. Some examples include having ultrasound procedures or portable X-rays done in the patient's room or a treatment room on the inpatient unit.
Inventory. This involves improving space utilization by reducing the amount of stored materials.
Utilizing an automated and secure system like those from Pyxis by Carefusion (www.carefusion.com) or Omnicell (www.omnicell.com) allows the supply chain to track inventory use, keep bulk inventory decentralized and stock daily with a just-in-time system. This frees up expensive storage space on the inpatient unit and in hospital support areas, so it can be used for patient care and staff support. A low-tech approach would be to provide modular storage systems in a way a modular closet system might be used in a home. This helps maximize the functionality of the storage space.
It also can be helpful to have the storage visible so that items can be found easily. Visibility also encourages organization and neatness. Utilizing wall-mounted wire shelving units and mobile wire shelving units that can bank against each other maximizes space. Most hospital systems use several sizes of plastic bins mounted to a peg board or placed on shelving units. While most hospital systems own thousands of these in bright colors, selecting clear bins can increase stock visibility and reduce surprises. Clear bins allow staff to know immediately when stock is running low.
Developing a standards master plan for furniture and interior finishes allows a hospital to maintain its facility easily and respond to equipping rooms with universal size and function. Standardized loose furnishings, such as those in patient rooms, allow health systems to replace damaged components or entire pieces easily. Modular desk and office components in standardized sizes allow reconfiguring universally sized support spaces quickly and easily.
With a standardized approach to finishes, staff can locate stored stock quickly or order the correct flooring material or plastic laminate, because finishes are all part of a well-documented kit of parts. When developing an interior standards master plan, health systems can pursue purchasing agreements with manufacturers that lower costs because larger quantities can be purchased as part of the standard plan agreement.
Many manufacturers are willing partners in committing to fabrication of identified standard material for an agreed-upon number of years — even if the product is discontinued as a part of the manufacturer's published offering. Many finish and textile manufacturers also are open to storing attic stock for large health systems and shipping it on an as-needed basis. Agreements vary from manufacturer to manufacturer, but some suppliers even will track inventory that they stock, notifying the system when inventory on one of their standards is running low.
A well-designed standards program can help keep inpatient units looking their best, increase maintenance staff efficiency and lower operational costs.
Motion. This calls for reducing movement of nurses and other clinical staff.
Shortening the path that nurses and other clinical staff must travel to serve patients is becoming a standard concern in health care planning. Decentralized nurses' stations can put the nursing staff and supplies immediately outside the patient room.
Another helpful concept is providing centralized, larger "hoteling" spaces or quiet rooms for staff to work in teams and/or focused work efforts. These hoteling spaces should have neutral names not related to a specific function to keep their functionality as flexible as possible. Constructing these centrally located areas with glass partitions or a partial-glass wall system increases visibility within the unit. For flexibility, facility professionals should consider installing a modular wall system instead of traditional hard-construction partitions. This greatly aids in reconfiguring the space for adaptive use.

Modular headwall systems with outlets mounted at comfortable heights minimize the need for nursing staff to bend over to reach outlets. The capital cost of a headwall system might appear to be more expensive initially, but the labor costs for plumbing and electrical installation are reduced. Additionally, if future renovations require additional gases or electrical requirements, the modular headwalls can be retrofitted and reconfigured for less cost and effort than outlets mounted directly into the wall.
Modular headwall systems also can offer a universal approach to patient rooms, keeping functions in the same place in each room, which further increases staff efficiency.
Waiting. This requires reducing the time spent between steps in the process.
Waiting to complete procedures and processes can be reduced by providing enough equipment and a decentralized location for most functions. Placing patient support areas in decentralized locations reduces the likelihood that nurses and other clinical staff will have to wait to use the computer, or to use a clinical service sink or piece of equipment.
Providing a point-of-care lab in the inpatient unit allows some routine lab testing to be completed without sending samples to the central lab. Most devices for this lab are handheld and only require data, power for recharging and an area for the devices to be placed.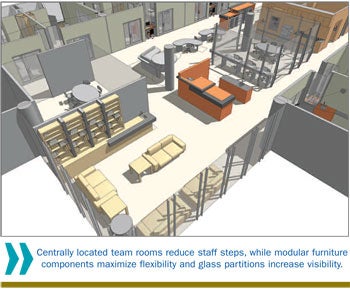
Planning for electronic medical records (EMR) in support areas to assist in scheduling patient procedures is critical. Accommodating such flexible casework systems as modular-component nurse
stations and physician work areas helps build in options for the transition to EMR systems over time. Because EMR often takes the form of wireless devices, handheld tablets and computers on wheels, EMR doesn't require as much traditional data port and countertop infrastructure.
Paper charting will be phased out over time. Offering flexible paper management systems for chart storage maximizes future reconfiguration opportunities.
Overproduction. This calls for reducing staffing inefficiencies caused by a lack of unit flexibility.
Planning an inpatient unit with decentralized support spaces based on an ideal nurse-to-patient ratio — typically 1-to-4 or 1-to-3, depending on acuity and hospital practices — disperses staff throughout the unit. Support space placed to maximize the ability to flex the patient load from one unit to another (or from a portion of the unit to another) increases operational efficiency, minimizing the need to maintain an entire unit for a few patients.
Likewise, lean options should be considered for surge capacity. Instead of programming the number of beds for the worst-case scenario, some units can flex to address a surge. For example, ED trauma rooms can be designed with double the required medical gas outlets.
Overprocessing. This involves overcoming reduced activity due to poor tool or product design.
Making the unit as adaptable as possible by not customizing permanent items and by standardizing mobile, modular solutions allows for adjustment of the work areas because of changing procedures or functions.
For example, by minimizing custom millwork cabinetry at nurses' stations or physician work areas, the millwork is kept very simple, allowing for flexible equipment such as file pedestals and other moveable accessories to customize the space. However, modular products, like systems furniture for nurses' stations, should be configured in ways that address the current requirements of a work area. This improves workflow for today and can change easily to adapt to new technology or processes tomorrow.
Defects. This requires reducing mistakes that can endanger patients as well as clinical staff.
Hospitals do not need to be brightly lit from top to bottom to have enough light. Enough light for a given function can be provided in cost-effective and energy-efficient ways by directing it on work surfaces through task lighting. To reduce eye fatigue, consider indirect lighting and personal controls in areas in which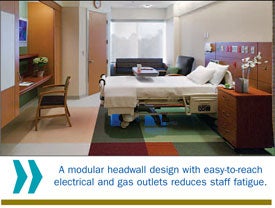 computer screens are used.
computer screens are used.
Consider cleaning and maintenance when selecting finish material to reduce operational costs. For example, providing waxless flooring can save maintenance requirements and costs, reduce the number of full-time equivalent employees and, more importantly, eliminate the cycle of waxing and stripping that produces toxic, indoor air quality.
By making the unit as lean and efficient as possible, the room, department or hospital should reduce staff fatigue, which also should reduce errors.
Improving functionality
Lean principles can aid in improving hospital functionality without requiring the redesign of entire departments.
This can be accomplished by reducing the movement of patients, staff and materials; reducing staffing inefficiencies; reducing customization; and helping to provide a safer environment.
Any one of these benefits has merit on its own, but coupled with operational savings, the principles of lean design are a compelling discipline for any health care organization to implement.
Brenda Smith, RID, IIDA, LEED AP, is senior associate and health care interiors team lead and Dawn Mixon Bennett AIA, LEED AP, is senior project manager, both at Perkins+Will, Atlanta. They can be contacted via their e-mail addresses at Brenda.Smith@perkinswill.com and Dawn.MixonBennett@perkinswill.com, respectively.




