Corridor hand-washing sinks and PPE cabinets between every pair of patient rooms at Yale-New Haven Hospital’s Shoreline Medical Center Surgery Center assist in infection prevention, including health care-associated infections.
Photo by Srey Sherman, Shepley Bulfinch
In early 2020, as the world shifted to managing the COVID-19 crisis, health care providers scrambled to understand how their facilities could safely absorb the surge of infected patients and prevent further illness among patients and staff. Now that it has been more than a year and a half of living with COVID-19, perhaps it is time to ask three fundamental questions:
- What is the appropriate level of capital investment for an event that may never again occur within the lifespan of existing and soon-to-be-built facilities?
- What if the next pandemic does occur in a decade or two but is substantially different in methods of transmission, virulence factors or other characteristics?
- Will designers have overplanned for COVID-19 and underplanned for whatever comes next?
Following is an overview of relatively modest design and architectural space planning considerations a pandemic-resilient health care facility might include to lessen the impact of future unknown pandemics, especially in the next few years before more definitive guidelines and standards are in use.
Owners, in consultation with their infection prevention and design teams, should become conversant with the technical definitions and distinctions between negative pressure, airborne infection isolation (AII) rooms and contact isolation to determine the number of each type for their facilities.
Reaction to COVID-19
Not all pandemics are created equal, yet designers seem to behave as though they are and either underplay the potential for disaster or overplay an architectural response.
These reactions to crises have precedent. After 9/11, there was limited focus on hardening emergency departments (EDs) against possible bioterrorism. Ebola gained significant media attention from 2013 to 2016, and several Ebola treatment centers were built in the U.S., most of which could handle a very small number of patients.
In retrospect, these centers may have been an overreaction to a threat that was not particularly acute in this country and may have distracted designers from the obvious and very real threat of a relatively contagious airborne virus that could easily infect, injure and kill hundreds of thousands of Americans.
Both the 2003 SARS and the 2005 H5N1 (bird flu) could have served as harbingers of the future — or perhaps because both caused what now feels like a small number of human fatalities in Asia, the design response was often limited to provisions for one or two floors of negative-pressure nursing units.
Now that the field has seen the impact of COVID-19 and the power of this virus, understanding the characteristics of this and other contagions (e.g., virulence, means of transmission, infection rates and communicability, and possible patient volume) and addressing how health care design can limit spread and support patients and caregivers merits attention as a precursor to design and capital investment.
Effective design solutions
The broad outlines of effective COVID-19 design solutions are fairly clear. In addition to providing more negative-pressure rooms and units, AII rooms, and individual patient care areas for contact isolation, separating care areas into infectious and noninfectious zones, limiting staff exposure to contagious patients, and providing staff with personal protective equipment (PPE) as well as appropriate respite spaces likely improves care for patients and safety for staff. Additionally, the ability to utilize exterior spaces for testing, patient sorting, respite and other functions proved beneficial to many.
Following are design solutions and concepts that architects may consider until more definitive guidelines are released:
Access and entry. Hospitals are now able to test for COVID-19 and separate patients and staff into infected and uninfected groups. Retrofitting and designing new lobby spaces with appropriate power, exterior and interior electronic signage, as well as waiting and staging zones (appropriately negatively pressurized, filtered, with cleaning, sanitizing and disinfecting systems) is recommended.
For EDs, the other hospital “front door,” enlarging all decontamination entry and support areas to support an influx of infectious patients is good practice. The key is designing these spaces so they can be fully utilized for noninfectious patient care once a pandemic has subsided. A second walk-in entrance for patients suspected of being contagious may be beneficial and should include space to assess and triage patients and families before they enter the department. If users can place an order at a drive-through restaurant, they should be able to communicate with the ED before exiting their cars and ensure that both patients and staff know what to do next.
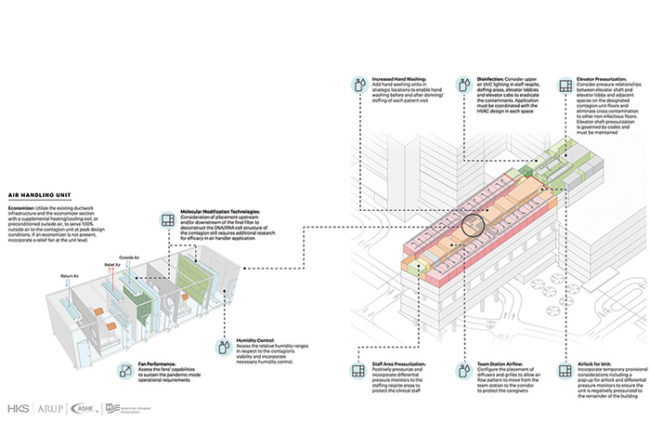
One-way flow. Conceptualizing patient, staff and equipment flows from clean to dirty may help determine where departmental vestibule and donning and doffing areas should be located and how clean and soiled depots should be supplied and emptied. This is three-dimensional and should include vertical as well as horizontal circulation systems. Even prior to COVID-19, some architects were designing soiled workrooms with direct access to a double-door elevator, allowing removal of soiled materials without passing through the elevator lobby.
One consideration for new construction is separating every elevator shaft into a single vertical element to eliminate the possibility of cross-contamination, with specific elevators designated for clean and others for soiled/infected materials and individuals. Although slightly more expensive to construct, there is an ongoing advantage in ease and safety of elevator maintenance.
Aggregation and “self-sufficient” compartmentalization. It is now clear that the typical practice of one or two AII rooms within nursing units, EDs (including behavioral health as its own mini department), and post-anesthesia care unit (PACU)/prep/recovery suites supporting invasive and interventional departments was inadequate to deal with COVID-19 in quantity and in practice.
Future best practice includes grouping a subset of patient rooms and patient treatment rooms into a negatively pressurized suite with staff access to medications, clean supplies, and soiled utility and equipment so that staff can treat patients without constant movement into and out of the area. In larger units, this model is unlikely to result in duplication of support rooms; in smaller departments — those with fewer than 12 to 20 patient care spaces — additional support rooms may be necessary to create a self-sufficient suite.
Point-of-care testing may need to be duplicated and distributed in larger departments. Whether or not these work areas should be enclosed will depend on the nature of the tests conducted and risks of aerosolization; though, as testing equipment becomes increasingly self-contained, open work areas may be sufficient.
Best practice also suggests that vestibules or anterooms (pressurized vestibules) that allow for staff hand-washing, donning and doffing should be designed as part of patient care suite entries and exits. Assuming the vestibule or anteroom is part of a corridor, adding 30 to 80 net square feet (nsf) off to the side for donning and a similar space for doffing may be sufficient. These areas may be utilized as storage or supply alcoves when donning and doffing are not required.
Consideration for staff respite (break areas) and individualized (socially distanced) dining either within or proximate to infectious patient care areas should be made, again, with the idea of limiting staff donning, doffing and travel out of areas with contagious patients.
Surgical, interventional and imaging. In addition to the compartmentalization of PACU/prep/recovery areas, is there still a place for patient care bays in preparation and recovery, given the lack of acoustical separation and possible source of bacterial contamination from cubicle curtains? From a space perspective, the difference between a patient care bay (cubicle curtains on two to three sides) and a cubicle (three walls and a curtain only at the footwall) is approximately 10 nsf, or 16 departmental gross square feet. A fully enclosed patient care room adds another 10 to 16 nsf and a sink over that of a cubicle.
- Anterooms to procedure and imaging rooms. Many hospitals are making more permanent the temporary negatively pressurized operating room (OR) anterooms erected during 2020 and are considering the creation of anterooms for interventional labs. Given the racetrack configuration of most OR suites, finding the best place for a permanent anteroom that does not impede circulation may be difficult. Most contemporary surgical services suites have been designed with the ORs arrayed around a centralized clean core, which means that either a second anteroom is required within the core or access between the core and “infectious” OR is eliminated, which is the option most owners are pursuing.
- Footprints for focused multivector ultraviolet and other disinfection units. There is likely to be a dramatic increase in the availability and effectiveness of these emerging technologies and, although their size may well decrease in coming years, current models are often the size of a patient bed and require a footprint of about 24 to 30 nsf. A reserved footprint should be determined within each space to be disinfected. It is unlikely to require additional square footage. Additionally, there should be an alcove-type parking space of the same size and dimension for each piece of equipment when not in use.
- Reading rooms for imaging. The trend shifting reading spaces out of the hospital has quietly accelerated in the past several years as hospital systems and demands for efficiency have grown. COVID-19 has increased this trend, and it is unlikely that there will be a return to full in-person reading capability.
Nursing units. Nursing units have the advantage of typically being capable of functioning as self-contained and self-sufficient entities when required to support contagious patients, although most could benefit from the addition of vestibules and/or anterooms for donning, doffing and one-way flow. Increasing the ability of some units to become negatively pressurized, as well as the number of AII rooms on units, will likely be a major issue for future construction.
Sliding doors have two great advantages for patient rooms: minimizing the disruption of air flow during opening and closing and effectively adding at least 16 nsf to the size of the room by eliminating door swing clearances. Floor tracks are difficult to clean and should be avoided.
Possible modifications to reduce direct staff exposure to infectious patients include cable portals that allow some equipment, such as monitors, to be connected to the patient but located in the corridor. These portals should be gasketed for corridor life safety and to eliminate air flow leakage from a contagious patient to the corridor. Determining which equipment may be safely operated remotely will require thoughtful review and testing of the cables, tubing and other elements.
The suggestion of widening corridors to 10 feet to support equipment relocated from the patient room to just outside the room has obvious advantages, although the space impact would be at least 32 square feet per patient bed (assuming a 32-foot structural bay); almost 800 square feet would be reassigned from net to circulation space with a 24-bed nursing unit. It is difficult to determine how this space could be used effectively when there is no pandemic, although furniture-based documentation stations just outside the patient room are one option.
In addition to improving visualization of patients, the ability to use portable radiography from outside the patient room was repeatedly demonstrated during 2020, although staff must still enter the patient room to position the patient before and after image capture. There is evidence that “smart” switchable glass does not significantly impact the quality of the image, but there may be minor backscatter radiation. Elimination of cubicle curtains merits consideration, though it triggers a chain of options to preserve visual privacy, such as knocking on solid doors, or the use of integral blinds or switchable glass in doors and windows in interior partitions, often called “borrowed lites.”
The concept of providing low-level return air ducts at the patient headwall to lessen the possibility of contamination, especially during procedures such as extubation, has the significant downside of requiring relatively frequent filter replacement due to the large amount of lint generated in patient rooms.
Turning to removable rather than fixed-room elements such as visitor sleeping couches and the patient wardrobe, so that, in the event of infectious occupants, the patient room can be stripped down, reduces both the possibility of contaminants remaining within and cleaning time.
Many hospitals, especially academic medical centers with rounding students going in and out of patient rooms, were reintroducing corridor hand-washing sinks and large PPE cabinets between every pair of patient rooms even before COVID-19. Sink alcoves should be large enough to allow for trash containers and provisions for hand drying.
Other considerations for nursing units include storage for the various robots (e.g., meals, medications, supply deliveries and retrievals, and virtual clinicians on an iPad). Alcove storage for mobile radiology equipment, especially in intensive care units, should be considered.
Programming a conference room (180 to 240 nsf) as flexible and convertible space in nursing units and procedural areas proved to be an asset in many hospitals. When located at the entrance of the unit, conference and/or office space became donning and doffing areas; when located at the center of the unit, these rooms served as supplemental supply areas or additional staff charting and workstations. Modifications to the conference space are minimal and likely to be no more than additional electrical and data outlets a minimum of every 72 inches, especially if corridor hand-washing sinks are located nearby.
Respiratory therapy. Both processing and storage requirements should be reviewed and most likely enlarged. Documentation and dry or computer workspace may also need to be reconsidered.
Storage and supply chain management. Just as most health care systems are rethinking their reliance on just-in-time supply chains, provisions for the storage of supplies from the loading dock and materials management, as well as within individual departments, deserve another review and game plan should there be another pandemic.
Added benefits
If there is a silver lining to the current situation, it is that the renewed dedication to infection prevention may continue to help health care facilities in their fight against health care-associated infections (HAIs).
Although tragically dwarfed by COVID-19 deaths, largely preventable HAIs in clinics and nursing homes as well as hospitals may decline due to the facility investments and design strategies used to combat a pandemic.